Our forward-focused conversation continues with this third installment in a series focused on Advancing Continuing Medical Education (CME*). Most recently, our article focused on team-based education and the importance of design. In this article, we will explore themes supporting a need to shift from single programs that target large audiences toward programs that reach a targeted group of learners in a more in-depth educational experience, where clinical gaps warrant. The examples of this can be vast and varied, from quality improvement projects to a focus on changing an educational climate or specific practice environment.
As a reminder, the themes and findings outlined here are part of research, done within our community, evaluating progress on the “20 predictions” for CME.1 Detailed project methodology can be found in the aforementioned two articles in this series. We encourage you, the reader, to view these findings in the context of your roles and responsibilities as well through your inclusion within the CME community.
Frameworks Geared to Complexities of Healthcare
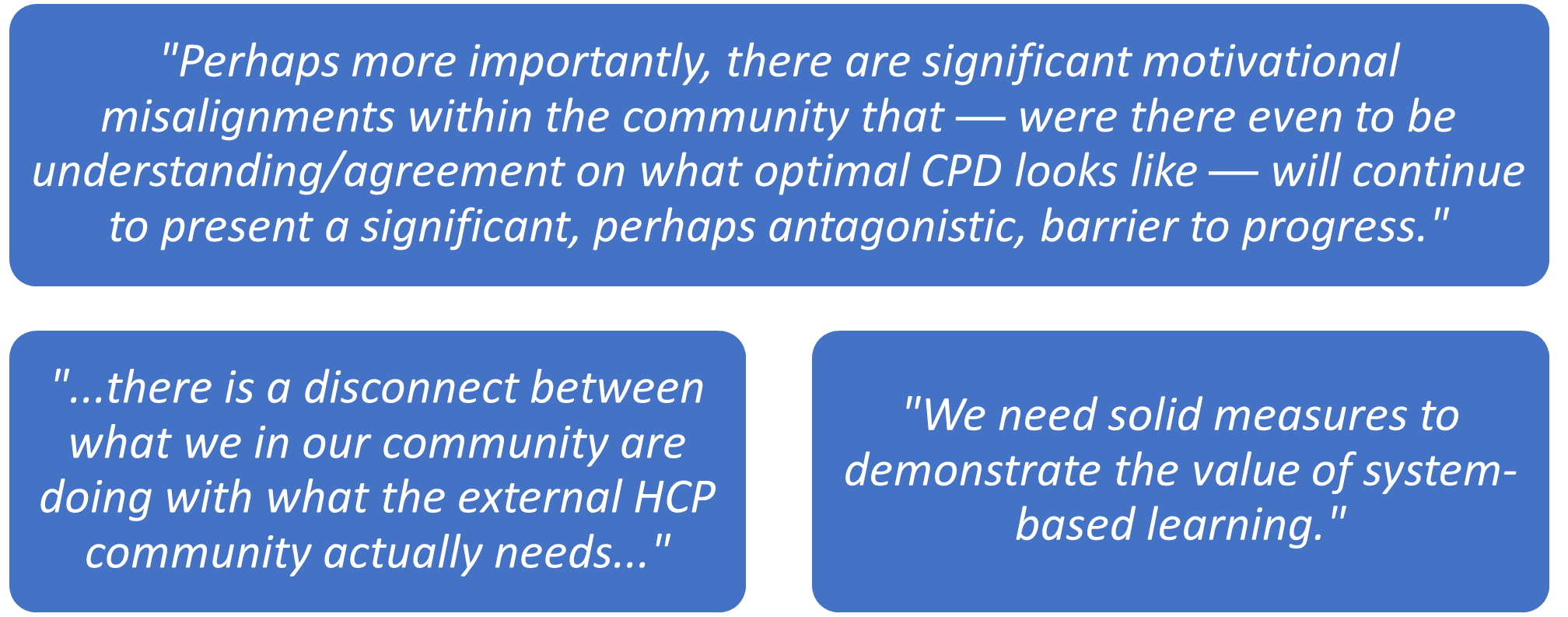
When asked to rank the most important themes for the future of CME, 67% of survey respondents chose “the adoption of evaluation frameworks that are better geared to the complexities of practice change within contemporary healthcare environments and the recognition of theory-based approaches” as their top answer. This is further supported by the following comments from respondents:
Complexity within healthcare drives practice gaps that are beyond the scope of a single individual.2 Often, the role of CME is to evaluate individual knowledge or competency change, focused on change following a single timepoint associated with an educational event. However, it is vital to consider the embedded drivers of practice gaps within these complex healthcare systems. A useful framework is the evaluation of practical barriers to care that are influencing variations in care, or variation from evidence-based care. How do systems and processes enhance or limit implementation of best practice? How does HCP preference drive decisions? What knowledge gaps exist? Are there incentives that drive care, and are those aligned to best practice? CME can help build competencies to navigate systematic change, internally and externally, leveraging different educational strategies to support environmental and practical change within healthcare.
Multidimensional and ‘Deep’ Education
One strategy to tackle the bridge between healthcare complexity and implementation science is the use of multidimensional education strategies. Unsurprisingly, survey respondents found this an important theme for the future of CME.3,4 Often this can involve healthcare system partnerships, longitudinal curricula, quality improvement programs, and other large-scale and deep-seated initiatives. These efforts are often more time consuming and resource intense but frequently lead to a prolonged and sustained practice change.
The fundamental constructs of multimodal, deep education dovetail beautifully with principles of implementation science. The focus becomes adaptation of an intervention through working with ground-level stakeholders. Buy in and scalability become the focus of adaptation. The successful alignment between complex interventions and implementation science can yield sustainable agents for change.4,5
Humans are heuristic by nature. When given the option, our brains will take a known successful path over the complexity of developing a new route. The overwhelming flood of published research, opinion pieces, and changing guidelines annually make it impossible for HCPs to stay up to date. It is natural and expected that humans, who are also HCPs, may shift some cognitive load toward reliance on systems to guide practice decision-making.6 Helping HCPs recognize individual gaps and heuristic thinking can be a critical element within a personalized continuing personal development plan.
Continued Call to Action
Understanding human behavior and the macro- and micro-complexities in healthcare can help shift the narrative on CME deliverables. The CME community holds the charge to continue creating change agents, exposing needs and gaps within the institution of healthcare, and focusing on purposefully moving the needle on understanding how educational content can advance HCPs along the learning continuum. We hope this series will foster self-reflection about how each of us can shift the narrative on CME deliverables.
*CME is used within this article to refer to accredited education for healthcare professionals, including CME and CE.
References:
1. Olson CA. Twenty predictions for the future of CPD: implications of the shift from the update model to improving clinical practice. J Contin Educ Health Prof. 2012;32(3):151-152. doi:10.1002/chp.21139
2. Plsek PE, Greenhalgh T. Complexity science: The challenge of complexity in health care. BMJ. 2001;323(7313):625-628. doi:10.1136/bmj.323.7313.625
3. Braithwaite J, Churruca K, Long JC, Ellis LA, Herkes J. When complexity science meets implementation science: a theoretical and empirical analysis of systems change. BMC Med. 2018;16(1):63. doi:10.1186/s12916-018-1057-z
4. Best A, Berland A, Herbert C, et al. Using systems thinking to support clinical system transformation. J Health Organ Manag. 2016;30(3):302-323. doi:10.1108/JHOM-12-2014-0206
5. Kitson A, Brook A, Harvey G, et al. Using Complexity and Network Concepts to Inform Healthcare Knowledge Translation. Int J Health Policy Manag. 2018;7(3):231-243. doi:10.15171/ijhpm.2017.79
6. Liang JJ, Tsou CH, Dandala B, et al. Reducing Physicians’ Cognitive Load During Chart Review: A Problem-Oriented Summary of the Patient Electronic Record. AMIA Annu Symp Proc. 2021;2021:763-772.
Check out more from this series: Part 1, Part 2 and Part 4.
Sarah Nisly, PharmD, MEd, BCPS, FCCP, is vice president, outcomes and clinical impact, within the Clinical Education Alliance.
Caroline Pardo, PhD, CHCP, FACEHP, is president, CPD, within the Clinical Education Alliance
Cody Ortmann is associate director, medical education grants & sponsorships, for Genmab.