This is the second article in a series, focused on original research that was first presented at the Alliance 2023 Industry Summit (AIS) session, “What’s next? Revisiting ‘20 Predictions for the Future of CPD’: Looking back to inform the future.” This article is focused on findings related to team-based learning and the relevance and importance of team-focused educational design. Future articles will be focused on other findings and implications from our primary research within the continuing professional development (CPD) community.
Evolution of ‘Team’ in CME*
In 2012, Dr. Curtis Olson, as the editor in chief of JCEHP, outlined a collection of evolving themes and areas of focus that he saw on the horizon for the CME landscape.1 These “20 predictions” attempted to forecast directionality and provide context for several emerging transformations within CME. To understand the current landscape of CME and perspectives of CME stakeholders, we gathered insights from a survey conducted among members of the CME community during April–May 2023. This was done to explore perspectives of CME stakeholders related to the potential evolution of future predictions, such as educational design or insights, that will be important over the coming decade.
Within the survey, we summarized eight statements from the original 20 “predictions” and asked survey respondents to assess the relevance of these various statement themes among our CME/CE community today. Three of the statements were related to team-based learning and team-focused education design.
Within the healthcare sector, the term "team" holds great significance. Often, “team” is used to denote the collaborative professional environment in which healthcare professionals operate. More formally, a team is a group of professionals who come together, leveraging their unique expertise, skills and perspectives to provide comprehensive and effective care to patients. This concept extends beyond professionals within a specific department or discipline, to encompass a multidisciplinary approach that includes doctors, nurses, pharmacists, allied health professionals, technicians, CPD administrators, support staff and others acting together toward a common goal: promoting patient well-being and achieving optimal health outcomes.
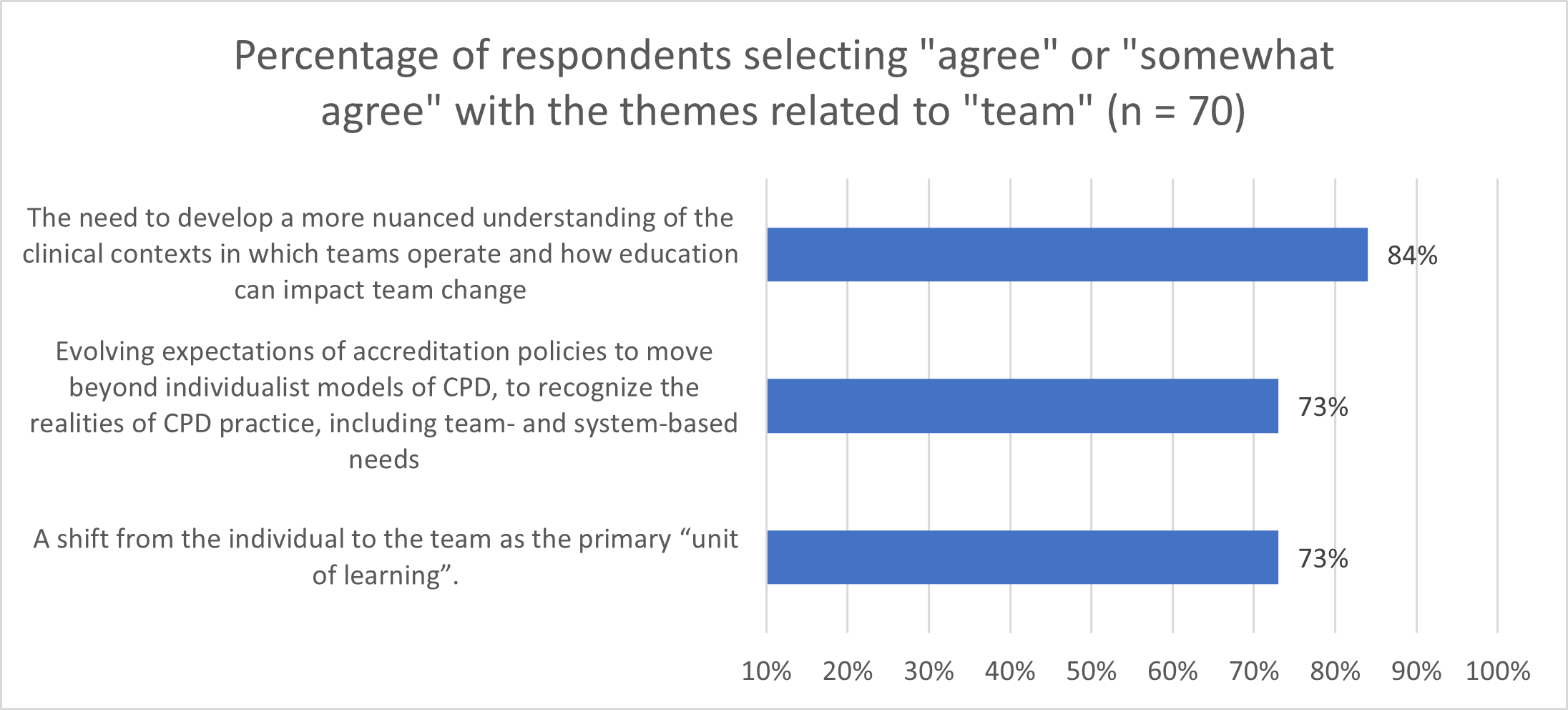
Amongst the respondents in our survey research (n=70), three-quarters indicated that the “team-based” statements remain relevant to our work in CPD today. [Figure 1]
After identifying relevant themes, survey respondents were asked to rank order the themes in order of importance. All eight themes were available for consideration and respondents were asked to select up to three responses.
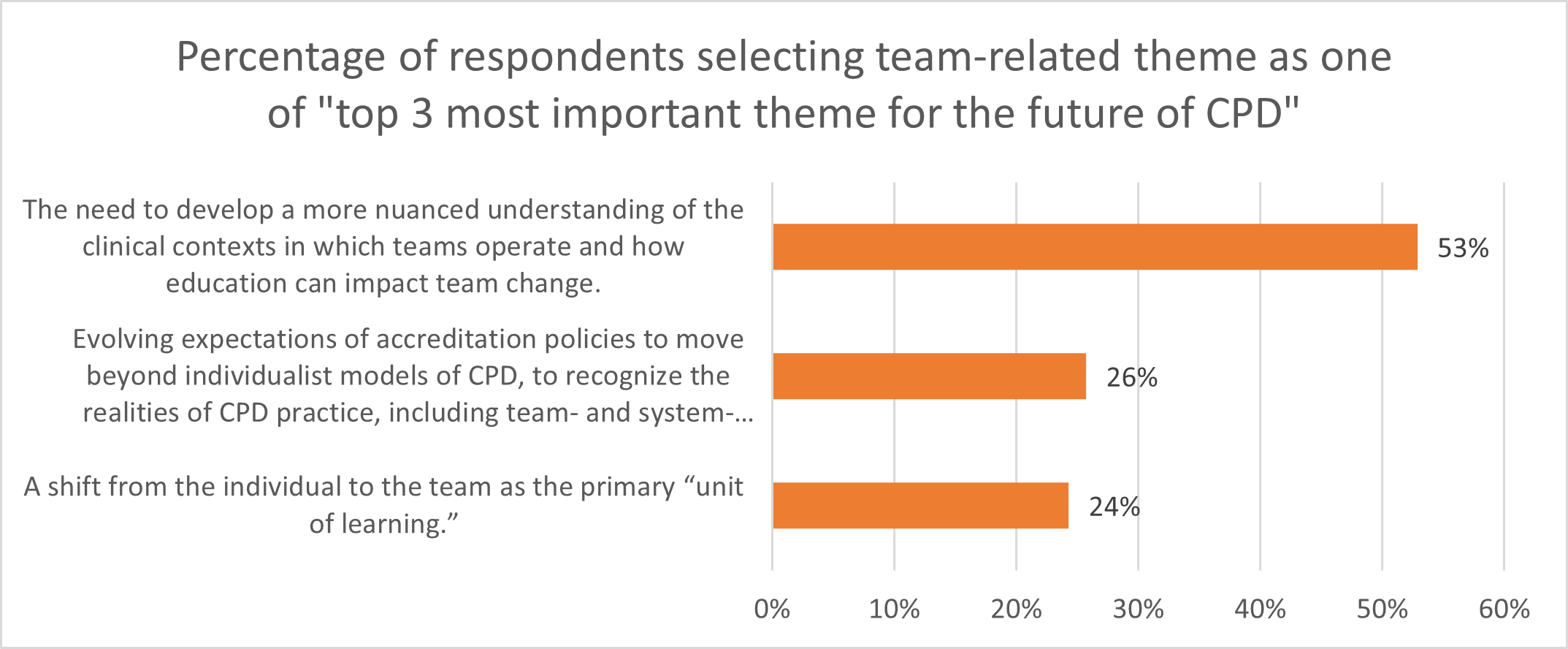
Over half of the respondents (53%) identified the following theme as among the most important for the future of CPD: The need to develop a more nuanced understanding of the clinical contexts in which teams operate and how education can impact team change.
Interestingly, the themes surrounding the realities of CPD, including team-based needs within accreditation policies and that are related to a shift from the individual to the team as the primary “unit of learning,” were identified commonly as important to the future of CPD. “Team” appears to matter because it is the context in which healthcare professionals work and, thus, is a critical factor that may serve to drive change or, conversely, create the context of inertia or resistance to change.
Qualitative commentary collected as part of this research describes the complexity of effectively designing CME/CE to meet underlying educational needs:
- “… in reality it is very challenging to design CPD interventions that can successfully interact/engage with and meet the needs of the different learners/specialists that might compose a specific clinical team.”
- “… healthcare decision-making is a teams-based approach, and … quality metrics (like the EOM) are calling for higher level focus on collaborative advancement. This needs to be explored.”
- “… programs that are grounded in decision science .... This may involve a mix of individual knowledge acquisition and team-level collaborative learning and practice change efforts, depending on the specific needs of the learners and the healthcare community.”
In summary, in education design, whether to focus education on individual healthcare professionals or teams is not an “either/or” choice: CME can and should be designed to address the underlying educational needs of HCPs in order to effectively address observed clinical gaps. As a community, we should question if we are using sufficiently robust and effective methods to determine the cause or drivers of clinical gaps, including consideration of whether those gaps are at the level of team performance or rather at the individual healthcare professional level. Addressing this question may serve as an impactful opportunity to advance research and understanding.
Too often, CPD programs may be too narrowly focused, such as by concentrating solely on specific aspects of patient management or emerging evidence, or by being tailored to a particular specialty group or degree type among the target audience. Unfortunately, narrow approaches fail to consider the multidisciplinary nature of patient care, which is crucial. Therefore, it is essential for our community to explore innovative and creative methods for identifying clinical care gaps, determining their root causes and ultimately finding the best strategies for improvement.
How should we appropriately identify the educational need we aim to address through education as being a team-based need, an individual healthcare professional need or both? We look forward to others’ contributions to this area of investigation and thought development.
*CME is used within this article to refer to accredited education for healthcare professionals, including CME and CE.
References:
- Olson C. Twenty predictions for the future of CPD: implications of the shift from the update model to improving clinical practice. J Contin Educ Health Prof 2012;32(3):151-152
Check out more from this series: Part 1, Part 3 and Part 4.
Caroline Pardo, PhD, CHCP, FACEHP, is president, CPD, within the Clinical Education Alliance.
Sarah Nisly, PharmD, MEd, BCPS, FCCP is vice president, outcomes and clinical impact, within the Clinical Education Alliance.
Dustin Ensign, CHCP, is director, medical education and research, within Grail, LLC.