Introduction
Workplace burden and professional burnout have been well documented among clinicians. More specifically, “burnout” is defined as “a long-term stress reaction marked by emotional exhaustion, depersonalization and a lack of sense of personal accomplishment.”1 However, these issues that are detrimental to job performance, well-being and personal satisfaction have not, to our knowledge, been studied in a population that serves continuing education/professional (CME/CPD) practitioners.
Most professionals who work in the CME/CPD environment know how multi-faceted, complex, challenging and, well, downright burdensome the work can be. We strive to provide continuing education for healthcare professionals that is relevant, engaging and unbiased, but keeping all the proverbial “balls in the air” can be challenging. Juggling accreditation standards, best practices for adult education and learning, staff and resource management, funding issues, federal, state and institutional regulations, and more can turn our work into a circus that hinders our job satisfaction and overall well-being.
With those issues in mind, the Alliance Research Committee conducted a survey of CPD professionals to determine exactly which burdens impact them the most, which are most prevalent and how these burdens impact delivery of CME/CPD content and the profession in general. We developed an open-ended survey that was deployed to the membership in the spring of 2019. The survey was organized into 10 themes, allowing members to identify if they experienced burdens within that theme and to state specifically what those burdens were. Within each theme, subthemes were categorized to determine the types of burden that constituted each theme. Subsequently, we shared our findings with Alliance members at the 2020 Annual Conference in a learning session titled, "Burdens and Barriers That Put CPD Professionals’ Well-being at Risk." Attendees provided commentary at our session on potential solutions to at least some of the burdens we describe here.
Results
A total of 464 responses were obtained (response rate = 17%). Respondents were primarily women (78%) between the ages of 51 and 75 (68%). Most reported working in the CME/CPD field for more than 10 years (60%) and work in hospitals and health systems, medical education companies (MECs), medical specialty societies or medical schools (78%). About one-third of respondents (30%) had either the Certified Healthcare CPD Professional or Healthcare CPD Associate certification.
Question 1 focused on the burden of funding. While almost 66% of respondents reported that funding is a burden, specifics ranged from the process involved in acquiring an external pharma or educational grant and a general lack of funds to rising external costs, politics and government regulations, as well as grants that are funded by multiple entities.
“We receive no institutional financial support (except the office space we live in).”
“Our group has to be financially self-sufficient and turn money back to the university each year. Not knowing how we will do each year creates anxiety.”
At the Alliance session, participants discussed possible solutions, such as the need for internal marketing and more physical “presence” for the CE office, based on the impression that the more an institution values the CE office, staff and professionals, the funding will follow.
The second question addressed staff. While 56% reported that staffing issues are a burden, specific responses reflected an understaffed CE office, staff’s lack of knowledge and expertise in CPD, lack of value from leadership, turnover and difficult recruitment, and the necessity for the CPD office staff to “wear many hats.”
“One-person (one FTE) program for the past 9 years despite 50% program growth - offerings and attendance.”
“I oversee the Education area and we have major staff turnover. I have at least one vacancy a year, and it can take upwards of 5 months to hire and then an additional 3-5 to train.”
Alliance session participants identified the following potential solutions:
- The need for more technology to simplify CE staff work
- The need for time with staff to address soft skills as well, as strategy and pressing needs
- Interaction opportunities within and across CE teams
Question 3 on the survey asked about regulatory burdens specifically invoked by governmental agencies. While 72.8% of respondents reported this was not a burden they experienced, some CPD professionals reported laws and regulations, such as Sunshine and Stark, were difficult to interpret, and that it was burdensome to stay current with regulatory changes. Reported regulatory burdens also appear to be more closely associated with state-specific regulations for CE, rather than federal or national requirements.
“Massachusetts domestic violence education mandate. Initially, MA encouraged approved CE providers to apply to have their curriculum approved. By the time we submitted the curriculum, MA developed its own course free-of-charge so our course was declined approval.”
“FL Board of Medicine is requiring an increasing list of education for licensure renewals. They are also limiting the providers of this education to select 'approved' groups. Even though we are ACCME-accredited providers, we are unable to offer our staff the required education.”
Alliance session participants identified educational resources and sessions at the Annual Conference that are more inclusive of all types of CE providers as possible solutions to regulatory burden. Each of our requirements is so diverse, finding a good educational session is difficult for many groups.
However, the burdens associated with accrediting bodies was a different story! Almost half (46.3%) of the 464 respondents reported burdens imposed by accrediting bodies. The top three complaints focused on challenges in complying with the ACCME’s criteria, the burden of documentation and the lack of harmonization among accrediting bodies. The complexity of various regulations, combined with lack of clarity in answers from the ACCME, spoke to the frustration that CPD professionals experience when trying to comply with rules from accrediting bodies.
“Inconsistent criteria across healthcare bodies, interpretation of the various criteria, simplified forms overdue”
“Some of the reporting for the ACCME in PARS has become burdensome. There seems to be a regular increase in the information that ACCME chooses to require to add an activity. The collection of data for boards has significantly increased that burden.”
Some complaints about accrediting bodies included suggestions for improvement, such as simplifying forms or harmonization of requirements. During the live session, attendees put the “burden” of improvement on the accrediting bodies and suggested that accreditors harmonize the kinds of outcomes desired from CE. When reacting to the question of burdens imposed by partners, comments became more intense. Nearly a quarter (23.9%) of survey respondents reported burdens caused by partnerships. CPD professionals mainly expressed a lack of trust with partners due to different interpretations of communications, and keen disappointment in partners not pulling their weight. A third, lesser area of complaint was how time-consuming the relationship could be. Several comments pointed directly to joint sponsor partnerships.
“If we have to train new partners, it is time-consuming. Addressing their CME-related questions can get in the way of doing real work.”
“Everyone wants [to be] paid the majority of the grant and yet wants to do minimal work and miss deadlines.”
Live session attendees suggested the following to address partner lack of trust:
- Set expectations upfront
- Communicate deadlines
- Engage in constant communication
- Have one primary point of communication with the partner
The burdens that surfaced regarding the external CPD environment were echoed in response to question 6 about the workplace environment. Comments here mostly focused on unattainable or unreasonable expectations from management, poor work environment, and a lack of understanding or respect of CME by the greater organization. Being tasked with “doing more with less” sums up many of the comments CPD professionals contributed to this area.
“Administration is rather hostile toward any request for CME assistance for clerical support.”
“Expected to consistently do the work of 2-3 people.”
Employees who are not in a leadership position are not empowered to change much about their work environment. Still, participants at the live session suggested that workplace environment improvement could happen in settings where offices were scattered across a campus with the use of technology to reduce distance and establish stronger communication.
Previous comments about burdens due to accrediting bodies and the workplace environment were repeated in Question 7 on administrative burdens. Although 56% did not consider administrative duties to be burdensome, 40.3% identified significant burdens due to paperwork, processes, financial reconciliation, accreditation requirements, lack of staffing and technology tools.
“Not enough hours in the day, week or month to accomplish administrative tasks required by the overall institution.”
“There is a large paperwork burden to our customers who want to host event. We don't have enough staff to do it all for them.”
Half of respondents do not consider technology as an issue with only 50% identifying technology as a burden. Prohibitive costs, lack of integrated learning management systems and technical challenges with existing equipment were the top difficulties shared. Interestingly, CPD professionals cited lack of comfort with technology as a concern not only with staff but learners as well.
“There does not seem to be a good 'out of the box' solution to the technological needs of a CME provider. There are so many moving pieces and so many different aspects that are unique to each provider that developing a solution for even something as seemingly simple as disclosure management can take significant time/resources.”
“We have no support, no budget and no champions for improving technology for CME.”
Possible solutions provided by session participants included:
- Request support from leadership by demonstrating a learning management system
- Project time and money spent on technology, when understaffed
- Obtain proper IT training for staff
Sixty-one percent of respondents identified outcomes as a CPD burden. Challenges enumerated include lack of access to data (including poor response rate with follow-up), lack of outcomes staff or tech resources, a need for standardized reporting and a lack of meaning with outcomes data. Other respondents felt unsure if they were measuring the correct outcomes or if their evaluations were structure correctly to assess gaps or meet accreditation criteria.
“Unless you are part of a closed system, there is no practical way to measure outcomes.”
“Besides evals and outcome measure surveys, it is dang near impossible to collect any other data for the outcomes portion of accreditation. I don't have access to the things the ACCME seems to require.”
Session participants offered the following recommendations in response to outcomes burden:
- Look for consistency in outcomes
- Identify standard questions to ask physicians to standardize outcomes
- Utilize survey software that is easy to use
- Seek training on how to create better survey questions
- Ask physicians to help interpret data
- Identify a third-party outcomes vendor to assist in improving outcomes data results
Relationships with colleagues were cited as a burden by 15% of the respondents, specifically around individuals who do not understand CME requirements, style differences between departments and generations, differing priorities within a workplace, stress/drama and being perceived by colleagues as a compliance officer.
“People refer to me as a compliance officer. They tend to believe that I'm misinterpreting ACCME requirements to make their lives more difficult.”
“I feel like a babysitter! Constantly have to ask, remind people to complete a task.”
Sub analysis showed us that burdens differed by section (Table 1).
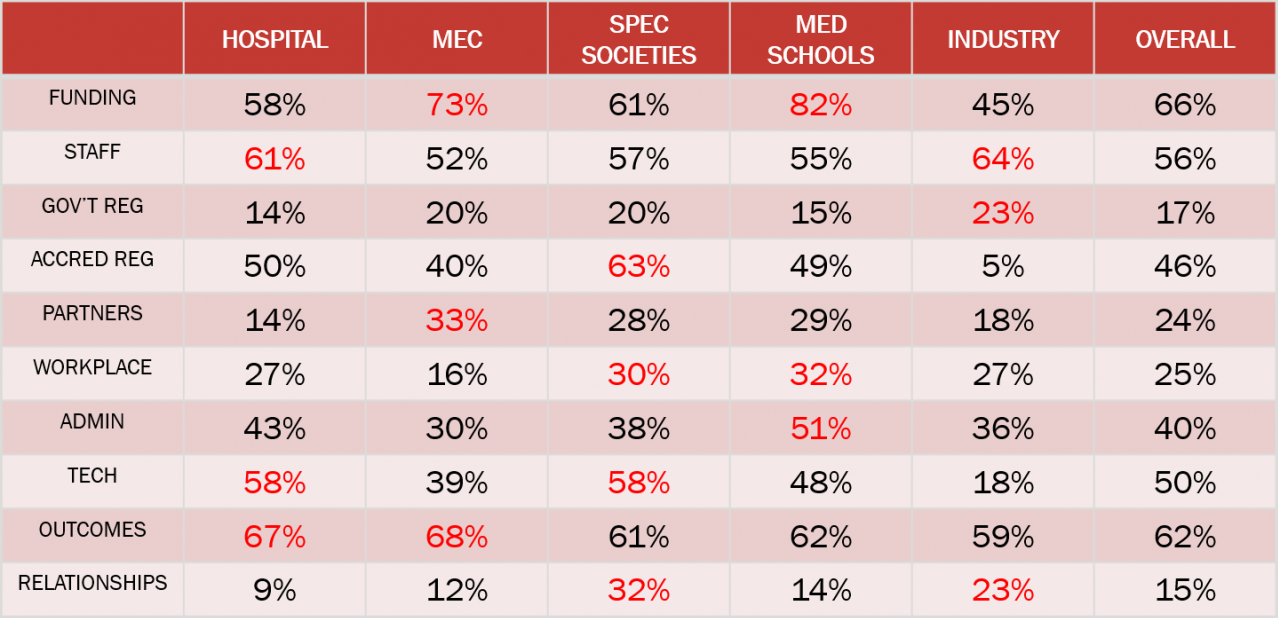
For instance, those in MECs were more likely than other sections to indicate burdens related to funding, partners and outcomes while those in industry were more concerned with staffing issues, government regulations and colleague relationships. Further work to alleviate burden should consider the different organizations in a diverse community, such as the Alliance, to ensure that our focus is both specific enough to be useful yet broad enough to engage and support all members.
Why Does All of This Matter?
We asked about the effect of these burdens on career plans. While half of respondents indicated that they had no effect, 9% indicated that they are planning to retire soon due to these reported burdens, 9% will change careers and 13% will seek a different job in this field. Further, we found that while job satisfaction was generally high, a greater number of burdens was inversely correlated with job satisfaction. In other words, the more burdens an Alliance member experiences, the less satisfied they are with their career. While this may seem obvious, if measures can be taken to reduce burden, it may support greater job satisfaction and reduce the potential for burnout. This in turn could help alleviate other specific burdens in the community, most notably staffing and workplace environment.
Postscript
The world has undoubtedly changed since findings from this research were presented at the 2020 Alliance Annual Conference. We realize that many of the burdens we report have been transformed or exacerbated beyond imagination. Indeed, findings from a recent focus group study conducted by Alliance staff and members of the Alliance Research Taskforce subsequently revealed barriers that, frankly, we had no reason to inquire about before February 2020. The COVID-19 pandemic has required rapid changes in the way departments and organizations administer their CME/CPD programs, present content, and interact with colleagues and the healthcare providers they serve. There is also now mounting concern about decreases in funding for most department across many healthcare institutions. Additional burdens reported by continuing education professionals in the post-COVID-19 era include maintaining quality of education offerings when required to change delivery platforms, while keeping CPD for providers relevant, and at the same time managing staff who now work remotely. Not to mention, all of this at a rapid pace
The Alliance Research Committee intends to continue exploring the CPD burdens of its members, and we appreciate the feedback provided, both through the survey research and the feedback at the live session at the Alliance Annual Conference this year.
Reference
- Physician Burnout. Content last reviewed July 2017. Agency for Healthcare Research and Quality, Rockville, MD. https://www.ahrq.gov/prevention/clinician/ahrq-works/burnout/index.html