Overview
As healthcare education strives to become more patient-centered, few approaches are as enduring or informative as long-term collaboration between medical education providers and patient advocacy organizations. This article outlines the foundational elements of patient-centered education and highlights lessons learned from Medlive’s multi-year collaborations with advocacy partners such as the Asthma and Allergy Foundation of America (AAFA), National Organization for Rare Disorders (NORD), the American Partnership for Eosinophilic Disorders (APFED) and others. These experiences show how sustained partnerships enable the design of continuing medical education (CME) programs that more accurately reflect evolving patient needs, driving measurable improvements in clinician knowledge and competence.
Reframing Patient-centeredness in CME
High-impact continuing education starts with a clear thesis: Clinician learning must be anchored in a deep understanding of patient needs. Although “patient-centered” is frequently cited as a guiding principle, it often remains an abstract or retrospective concept. Truly patient-centered education requires ongoing, proactive engagement with patient perspectives and a structured process to ensure those perspectives shape clinician education from the outset.
Through multi-year collaborations with AAFA and other patient advocacy groups, Medlive has developed a model that embeds patient perspectives directly into the educational process. This approach recognizes that integration must begin well before content development, considering patient insights essential to program planning so clinician learning aligns with real-world care.
This model includes:
- Annual meetings with advocacy and clinical experts to align on themes.
- Pre-program focus groups and surveys with patients and caregivers.
- Deep advisory discussions with recognized clinical faculty experts and patient leaders to define clinical and humanistic gaps.
- Tethered education models linking clinician and patient-facing learning experiences
- Post-program assessments incorporating quantitative and qualitative insights.
This article outlines the essential components of this model — and illustrates what becomes possible when programs are developed with sustained patient partnership at their core.
Sustained Collaboration That Drives Insight
Establishing “patient-centered” as a strategic design discipline requires long-term investment in relationships with organizations that know those needs best. Overall, between 2020 and 2024, Medlive’s collaborations with AAFA contributed to over 50 educational activities, that addressed new approaches/understanding of allergic and atopic diseases with shared inflammatory pathways — conditions affecting overlapping populations and requiring coordinated, multidisciplinary care. Overall, about 38,000 clinicians and 12,000 patients and caregivers participated in these important educational programs. What distinguishes this model is its use of an iterative insight loop: Patient and caregiver experiences surface through partnership, which shape learning priorities, content design and outcomes measurement for clinician-targeted activities.
Kenneth Mendez, President and CEO of AAFA shares the impact of this approach, “We’ve seen time and again that the best educational outcomes happen when we engage early, plan collectively, and stay connected throughout the patient journey. Sustained collaboration invites diversity of thought, resulting in education that is evidence-based, real-world grounded and truly patient-centered.”
Tracking the Evolution of Patient Needs in Allergy and Asthma
What makes this approach effective is not merely the inclusion of patient voices, but a sustained, longitudinal commitment to understanding how those voices evolve.
Patient insights collected revealed a remarkable shift in patient perspectives — from confusion and disengagement to empowerment and informed participation and health journey engagement:
- 2021: Patients reported low awareness of their conditions, limited understanding of available treatment options and frustration with fragmented care.
- 2022–2023: While disease understanding improved, patients continued to report challenges with clinician communication and voiced concerns about the safety of new treatments.
- 2024: Patients and caregivers described themselves as informed and engaged in their care, expressing greater confidence in communicating with providers and advocating for treatment preferences.
These evolving insights and feedback from AAFA members (patients/caregivers) through focus groups and in-depth interviews directly shaped our educational priorities and content. A defining feature of these programs was their grounding in real-world patient insights, reflecting that education today must be as much about partnership and dialogue as it is about data. The education incorporated patient perspectives and emphasized treatment challenges, communication barriers and quality-of-life concerns that clinicians encounter in everyday practice:
- 2021:The pathophysiologic connections across allergic conditions.
- 2021-2024: Evidence-based criteria for treatment selection
- 2022-2023: Techniques for aligning care with patient goals through improved communication and approaches to patient communication regarding treatment and treatment safety. Strategies for achieving symptom control and enhancing quality of life.
- 2024: Models for integrated, team-based care coordination.
Impact Through Educational Gains
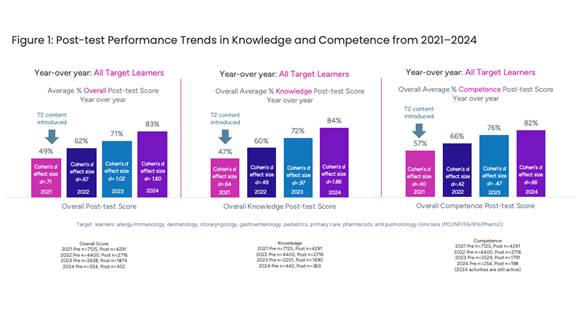
From 2021 to 2024, these clinician education programs demonstrated consistent and meaningful improvements in clinician knowledge and competence related to allergic and atopic conditions. Scored pre and post-test multiple choice questions were used to assess knowledge and competency, 5-point Likert scale evaluated pre and post confidence, and intent to change was reported via multiple choice and open-ended post-test evaluation questions. In some cases, behavioral changes were further characterized during interviews.
During this period, among clinicians:
- Overall post-test performance rose from 49% in 2021 to 83% in 2024.
- Knowledge gains increased from 47% to 84%.
- Competence scores improved from 57% (2021) to 82% (2024).
- In 2024, 94% of learners reported moderate to high confidence in shared decision-making.
- In addition, many participants cited planned practice changes, particularly around improving patient communication and tailoring treatment strategies.
While multiple factors contribute to educational impact, the sustained integration of patient perspectives help align content with the clinical realities and motivations of learners, contributing to the overall effectiveness of the programming.
Implications for the CPD Field
Throughout the multi-year collaboration with AAFA adapting and refining the patient-centered education model and process we identified several guiding principles emerge for the CPD community:
- Start with insight, not assumptions: Build insight collection into program planning, not just evaluation, and shape the learning objectives and the education accordingly, so that clinical teams can uncover ‘aha’ moments and patients and caregivers, access strategies to address their real-life challenges.
- Design for practical relevance: Focus on the real decision points clinicians face when addressing unmet patient needs, providing actionable strategies and resolving misalignment in treatment priorities to better address unmet patient needs.
- Measure with intention: Track learning outcomes that reflect the competencies required for patient-aligned care. Use the findings to generate insights that, combined with ongoing conversations with advocacy partners and their members, will shape and strengthen the next wave of programs.
As care models grow more personalized, the responsibility of CPD programs is not just to convey the science but to do so in ways that reflect the priorities and lived experiences of those receiving the care.
Conclusion: A Blueprint for Patient-aligned Education
Incorporating the patient voice isn’t a finishing touch — it’s a foundational strategy. Medlive’s experience across multiple partnerships illustrates how a structured, insight-driven model can elevate clinician knowledge and competence in ways that reflect the realities of patient care.
Organizations that invest in durable, authentic relationships with patient groups will be best positioned to design education that resonates — because they will understand not just the medicine, but the people it serves.
Leveraging patient insights enables us to develop not only relevant patient education but also clinician education that meets the real-world needs of both patients and clinicians, in order to improve patient care and health outcomes.
“I want to have an open discussion and forum with my doctor and my allergist about whether this medication will be beneficial for me, and I want to feel educated and empowered when I'm talking to them as well. I am an advocate for health equity within my patient community, and having access to patient-centered education online makes it all the more accessible for a lot of different ranges of patient types. I want to thank you guys for having such a big role in creating online patient education because it truly means so much to patients like me."
— Shreaya, Asthma Patient Advocate and AAFA Ambassador
Disclosure: This content was authored by a human with the support of AI tools for editing, summarizing open-ended patient feedback and referencing publications related to patient-centered education design.
 Carole Drexel, PhD brings over 20 years of experience in scientific research and medical education leadership. As vice president of medical education at Medlive, she designs innovative educational interventions to help close health care gaps and measure impact across a range of therapeutic areas. Drexel’s educational strategy leverages collaborations with academic institutions, professional societies, health systems and patient advocacy groups.
Carole Drexel, PhD brings over 20 years of experience in scientific research and medical education leadership. As vice president of medical education at Medlive, she designs innovative educational interventions to help close health care gaps and measure impact across a range of therapeutic areas. Drexel’s educational strategy leverages collaborations with academic institutions, professional societies, health systems and patient advocacy groups.
She previously held leadership roles at Global Learning Collaborative (fka The Omnia-Prova Education Collaborative) and Rockpointe Corporation, where she directed outcomes research and scientific strategy. Dr. Drexel held postdoctoral positions at The Johns Hopkins University School of Medicine and Heinrich Heine Universität.
She is an award-winning investigator and seasoned author with well over 50 publications in peer-reviewed medical, research and medical education journals, along with presentations at major medical conferences.
 Maria Arnone is the vice president of digital education at Medlive, where she leads with a passion for integrating science, technology and instructional design to improve patient outcomes. She specializes in building bridges between supporters, patient advocates and clinical experts to deliver credible, high-impact educational programs.
Maria Arnone is the vice president of digital education at Medlive, where she leads with a passion for integrating science, technology and instructional design to improve patient outcomes. She specializes in building bridges between supporters, patient advocates and clinical experts to deliver credible, high-impact educational programs.
Arnone has spearheaded the development and successful execution of digital education initiatives for both healthcare professionals and patients. Her strategic insights and collaborative leadership have helped secure program acceptance at leading scientific conferences including AAN, ASCO, ASH, ATS and AAAAI.
Previously, Arnone served at the American Academy of Family Physicians, where she gained formative experience in the continuity of care and the vital role of patient-centered education in family medicine.
 Nicolette Theriault, MPH is an outcomes analyst and researcher at Medlive, specializing in data collection, analysis and interpretation; translating data into a story. She is passionate about advancing medical education and improving patient health outcomes through evidence-based research and analysis.
Nicolette Theriault, MPH is an outcomes analyst and researcher at Medlive, specializing in data collection, analysis and interpretation; translating data into a story. She is passionate about advancing medical education and improving patient health outcomes through evidence-based research and analysis.
Her diverse background includes health programming, research, project management, medical writing, and publications. Theriault earned her BA in public relations and fine art from Quinnipiac University and her master’s in international public health from the University of Liverpool in the U.K.
 Nancy Paynter, MBA is a seasoned biopharmaceutical leader and strategist with over 25 years of experience at the intersection of commercialization, patient-centered care and tech-enabled innovation. She currently serves as strategic advisor to Medlive, shaping the company’s digital education strategy to better support healthcare decision makers. Paynter also advises life science companies, medical education providers and digital health startups on driving business impact through innovation in medical affairs and digital engagement.
Nancy Paynter, MBA is a seasoned biopharmaceutical leader and strategist with over 25 years of experience at the intersection of commercialization, patient-centered care and tech-enabled innovation. She currently serves as strategic advisor to Medlive, shaping the company’s digital education strategy to better support healthcare decision makers. Paynter also advises life science companies, medical education providers and digital health startups on driving business impact through innovation in medical affairs and digital engagement.
Previously, Paynter was senior director of global medical affairs strategy, planning & insights at Gilead Sciences, leading enterprise-wide strategy and performance initiatives across oncology, virology and inflammation. Before that, she spent 16 years at Genentech in leadership roles spanning medical education, system-based learning and community-engaged research — earning recognition as Manager of the Year. Earlier positions at Pfizer and PwC further shaped her expertise in strategic marketing, managed care and commercialization.
Paynter holds an MBA in Marketing and International Business from NYU Stern. She is CHCP-certified and a frequent contributor to thought leadership in medical education and patient engagement.