“I will always ask if the patient feels safe at home.”
“I’ll incorporate red flag questions into every patient interview.”
“This helped me think differently about what trafficking can look like in a clinical setting.”
These were just a few of the powerful comments and takeaways shared by healthcare professionals who attended the 2024 Human Trafficking Conference hosted by Western Michigan University, Homer Stryker MD School of Medicine (WMed) in Kalamazoo, Michigan. Held on Feb. 29, 2024, the interprofessional continuing education event blended didactic presentations from experts in the field, real-world cases and simulation-based learning to better equip frontline providers with the resources and confidence to intervene when human trafficking is suspected. The simulation-based learning was conducted at WMed’s Simulation Center, with cooperation from the center’s staff.
Research
Simulation-based education has been shown to significantly improve clinician competence, specifically in more sensitive areas such as trauma-informed care and human trafficking response. Studies have found that experiential learning strategies like simulation increase retention of complex communication skills and enhance provider confidence in high-stakes encounters (Kellerman & Heron, 2017; Gaba, 2004). In fact, simulation allows learners to safely engage with emotionally charged scenarios, making it particularly effective for training providers to recognize signs of trafficking and respond appropriately.
Additionally, interprofessional education (IPE) is increasingly recognized as a key driver of patient safety and systemic responsiveness. The World Health Organization (2010) has emphasized that IPE, where learners from multiple professions learn with, from and about each other, can lead to better collaboration and health outcomes. When addressing issues like human trafficking, where identification and intervention often depend on team-based effort, the integration of IPE and simulation offers a powerful, evidence-informed model for continuing education programs.
Why This Matters
Healthcare professionals are often among the few individuals with direct access to human trafficking victims. Yet, many lack training in how to recognize the signs or safely intervene. This conference aimed to close that gap, bringing together physicians, nurses, social workers, community leaders and others for a high-impact session that blended education with action.
With over 90% of participants rating the activity and presenters as “Excellent,” the conference made a strong impression. But beyond satisfaction scores, its most profound impact was seen on participants’ planned changes to clinical practice and their confidence in making those changes.
From Awareness to Action
Participants left the event with solid, obtainable goals:
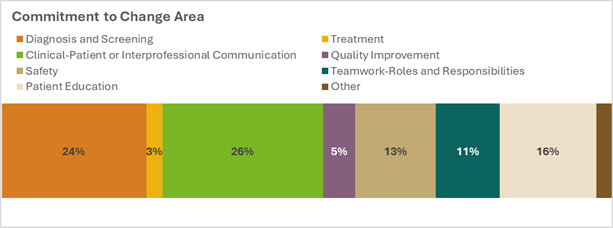
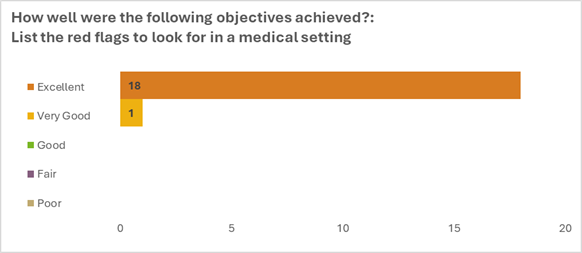
- Screening and Identification: 94.7% of attendees said they could now list red flags and describe effective intervention techniques. Nearly a quarter committed to improving diagnosis and screening, with one attendee noting, “I’ll ask about tattoos as a conversation starter — it may reveal more than you’d think.”
- Interprofessional Communication: 26% of participants planned to strengthen collaboration across care teams. One attendee shared a plan to create a mini-CE session workshop at their workplace to ensure all roles, from front desk to providers, understand how to flag and respond to trafficking.
- Patient Education and Advocacy: 16% aimed to better educate patients and provide resources in a trauma-informed manner, emphasizing safe, nonjudgmental environments. One respondent noted, “It’s about offering resources when they’re ready, not pushing, but making help visible.”
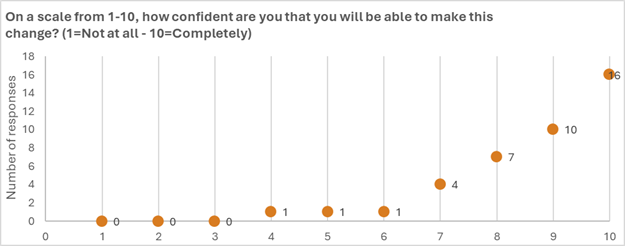
Confidence Matters
Of those who outlined specific practice changes, more than 90% rated their confidence to implement change at eight or higher on a 10-point scale. This boost in self-efficacy is no accident. The conference’s use of simulation scenarios — which featured WMed Simulation Center actors portraying patients and families — allowed participants to rehearse difficult conversations, make mistakes safely and receive supportive feedback.
One attendee said it best: “The simulations were invaluable. Memorable. I now know how to safely separate a patient from a potential trafficker and what language to use.”
Lessons Learned and Looking Ahead
This case study from WMed demonstrates that continuing education can go beyond knowledge transmission. It can transform clinical culture and behavior. When equipped with empathy, concrete strategies, and local resources, providers become powerful in the fight against human trafficking.
Key Takeaways:
- High-quality, simulation-based education improves both awareness and action.
- Interprofessional collaboration is essential. All team members need tools to identify and respond.
- Confidence-building is critical. Safe spaces to practice and to make mistakes lead to stronger real-world performance.
Next Steps
Interested in launching a similar program? Consider integrating role-play scenarios, local resource mapping and interprofessional dialogue. Above all, create space for reflection, as change begins with awareness, but it sticks with practice.
References
Gaba, D. M. (2004). The future vision of simulation in health care. Quality and Safety in Health Care, 13(suppl 1), i2–i10. https://doi.org/10.1136/qshc.2004.009878
Kellerman, R., & Heron, S. (2017). Trauma-informed medical education and practice. Academic Medicine, 92(8), 1051–1052.
World Health Organization. (2010). Framework for action on interprofessional education and collaborative practice. Geneva: WHO.
Disclosure: The use of artificial intelligence is acceptable for Almanac publications. The author utilized AI to fix grammar and phrasing and to double check against the rubric.