An Educational Initiative to Improve Atrial Fibrillation Diagnosis and Management
Atrial fibrillation (AF) is the most common cardiac arrhythmia worldwide and a leading cause of stroke, heart failure (HF), cardiovascular (CV) morbidity and sudden death. The global prevalence and incidence of AF are increasing steadily, particularly in developed countries, and associated increases in morbidity and mortality have been noted.1 Diagnosis of AF is challenging because brief or intermittent episodes are easy for clinicians to miss, and AF may produce mild symptoms that patients do not associate with heart problems.2 Importantly, one-third of all patients with AF do not experience any symptoms and are not aware that they have the condition.2-4 The disturbing prevalence of undiagnosed AF presents a clinical challenge because patients with the condition have a five-fold higher risk of developing stroke and a two-fold higher risk of death from stroke.5 Oral anticoagulation therapy reduces the risk of ischemic stroke by up to 70% in patients with AF, but undertreatment, driven in part by underdiagnosis, remains a major clinical challenge.6-9 This article presents a way to meet this challenge through the collaboration of the Heart Rhythm Society (HRS) and Haymarket Medical Education (HME).
HME designed a multifaceted CME/CE curriculum utilizing an approach that featured a mix of virtual meeting technology, mobile-optimized online activities and behavioral intelligence to geo-target, engage and address key educational gaps among clinicians and patients.
HRS was instrumental in developing a series of patient education resources that were designed to improve knowledge among individuals with or at risk for AF. By banding together, the two organizations were able to create a unique and innovative initiative to foster engagement among both patients and providers as well as increase knowledge of AF — including its symptoms, warning signs and available treatment options — while utilizing state-of-the-art geo-targeting technology to ensure that the right learners were reached at the right time.
Educational Design
The educational initiative consisted of three components:
A live myCME Town Wall™ video-based CME/CE activity: The myCME Town Wall is an innovative meeting technology platform that transports multiple faculty to a virtual stage, integrating face-to-face, dynamic communication among an in-studio moderator, on-the-wall faculty and learners participating remotely.
Use of this exclusive technology allowed for a greater number of participants on the virtual stage than would have been possible via more standard platforms, which provided for a multitude of perspectives and ensured that all perspectives were represented in the forum. As learner engagement is crucial to the success of any educational initiative, the Town Wall format was utilized to connect learners to the expert faculty panel, as though they were sitting in the audience of an actual roundtable discussion, providing a depth of interactive discussion and potential learning and reinforcement that cannot be captured by standard video technologies. Use of the Town Wall platform offered learners the opportunity to participate in an educational activity with the expansiveness of Grand Rounds from the convenience of their home or office. To extend the reach of the activity, the one-hour live myCME Town Wall was recorded and endured on myCME.com, the education portal of HME, for one year.
A CME/CE web-based myCME Case Clinic™: This online activity provided learners with the opportunity to revisit the foundational principles presented in the myCME Town Wall and provided evidence-based guidance on the integration of new knowledge into real-world clinical practice.
Participants in the accredited activities were invited via traditional myCME recruitment methods that included use of behavioral data, third-party data, dedicated email campaigns, smartphone push-notification system and the HME medical networks products suite.
Also utilized in recruitment efforts were HME’s unique Innovision products, myCME LIVE and myCME ENGAGE. LIVE utilizes a multichannel recruitment approach to penetrate and engage with targeted audiences; clinicians outside of the Haymarket Medical Network were reached through social media platforms and ad networks such as Twitter, Facebook, Google AdWords and LinkedIn. ENGAGE utilizes a similar multichannel recruitment approach to penetrate and engage with targeted audiences that include not only clinicians but also patients/consumers.
Non-accredited Activity for Patients
A patient and clinician mobile-based, geo-targeting initiative and patient education program: To raise awareness of the burden of undiagnosed NVAF and practical strategies for stroke prevention, this segment of the initiative was targeted to myCME Town Wall and Case Clinic participants as well as to patients who may be at risk for NVAF.
Approximately 90,000 verified mobile IDs of healthcare providers (HCPs) and patients were targeted. Selected individuals were sent a mobile ad asking whether they were aware of their potential risk for stroke: “Are you aware of the risks factors for AFib?” and “Stroke: Are you at risk?” To learn more about stroke risk factors and prevention strategies, the targeted individuals were invited to a dedicated patient education website — GetStrokeSmart.com — that featured a series of materials designed and selected by HRS to educate patient visitors about NVAF and its relationship with stroke.
Educational Aims
The overall learning objectives of the CME/CE components of the initiative were:
- Describe the magnitude of undiagnosed NVAF, including associated risk factors and the clinical and cost implications
- Initiate suitable screening protocols for patients at risk of developing NVAF and for those who may have silent AF
- Participate in individualized treatment planning and administration of care, which is guided by the most up-to-date management practices and informed by clinical evidence
- Implement collaborative care models to improve patient care, including a comprehensive approach to shared decision-making (SDM)
The initiative’s aims were focused on practical, interprofessional strategies to improve care for patients with/at risk for NVAF:
- Increase awareness of the magnitude of undiagnosed NVAF and raising the index for suspicion within healthcare teams, especially related to patient risk factors
- Equip HCPs with the education/tools they need to facilitate identification of undiagnosed NVAF and ensure that impacted individuals receive timely access to effective stroke-prevention medications
- Improve multidisciplinary collaborative strategies for coordinating aspects of care across multiple settings and for engaging patients in SDM
- For the Patient Education Program: Provide resources for HCPs and their patients with NVAF; expose patients with/at risk for AF to the HRS tools and resources
Outcomes Methodology Design
Pre-/post-activity surveys, program evaluations and eight-week follow-up surveys were used to measure changes in CME/CE activity participants’ awareness/knowledge (subjective and objective), changes in competence (subjective and objective), changes in self-reported performance (subjective) and to identify barriers to ideal performance.
For the patient component, the number of visitors to GetStrokeSmart.com were documented, as were responses to both the initial, introductory survey and a brief exit survey that asked patients whether they intended to speak with their clinician about their stroke risk.
Summary of the Initiative Outcomes
Participation in the myCME Town Wall live, Town Wall enduring and myCME™ Case Clinic activities exceeded expectations. Specifically, for the myCME Town Wall activities, 5,456 unique learners participated, in contrast to 2,650 anticipated. For the myCME Case Clinic activity, 4,803 unique learners participated vs. 1,250 anticipated.
Across all CME/CE components, significant improvements were documented in learners’ knowledge, competence and performance relative to the activity learning objectives.* For example:
- The percentage of learners who knew the patient characteristics/conditions that favor the use of direct oral anticoagulants (DOACs) over warfarin for stroke prevention in patients with AF increased from 22% to 85%
- The proportion of learners who knew that there are numerous potential advantages to detecting AF in an asymptomatic stage increased from 58% pre-activity to 98% post-activity
- The proportion who knew that real-world data show a reduced risk for bleeding with apixaban vs warfarin increased from 41% to 95%
*Based on 1,941 pre-activity and 1,792 post-activity responses.
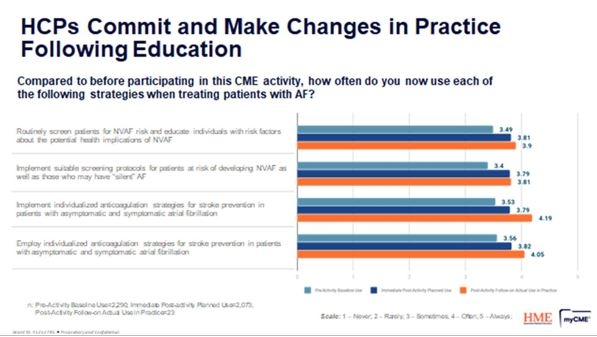
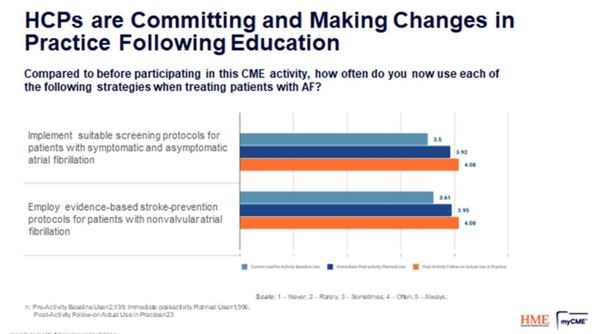
Participants in both the myCME Town Wall® and myCME Case Clinic components indicated that they planned to more frequently implement several suggested practice strategies following the activity vs baseline assessment. Results from a follow-up survey sent to learners eight weeks following their participation showed that participants did, in fact, implement these strategies more often than they did prior to participation.
myCME Town Wall® (live and enduring)
myCME Case Clinic
Across both components, it is estimated that the education may potentially impact the care of 45,065 patients with or at risk for NVAF each week.
Patient Education Program
Google Analytics data showed robust participation in the Patient Education Program among individuals at risk for AF/stroke.
- 4,400 total visits to GetStrokeSmart.com were documented; 1,002 of these visitors were HCPS, and 1,926 were patients.
- Visitors spent an average of 11:47 minutes engaging with content on the site.
- Compelling content drove repeat participation, with 19.4% of clinicians and 17.4% of patients making return visits.
- Real-world patient data, collected around the time of these activities, suggests that 7% of learners (n=78) participating in endured activities had a median volume of 327 patient encounters (range: 11-3008) over a 12-month period, based on ICD diagnosis claims.
Remaining Practice Gaps
Despite the documented improvements in knowledge, competence and performance, a number of gaps remain that require additional educational focus.
- At the conclusion of the myCME Town Wall® activity, nearly 30% of learners still did not know that people with asymptomatic AF had an increased risk for CV and all-cause mortality, compared with those with typical AF symptoms.
- Nearly half of myCME Town Wall participants (43%) still did not know that oral anticoagulation therapy to prevent thromboembolism is recommended for all male AF patients with a CHA2DS2-VASc score of 2 or more and in all female AF patients with a CHA2DS2-VASc score of 3 or more.
- Almost 35% of myCME Town Wall learners still did not know that real-world data showed a decreased risk for bleeding with apixaban vs warfarin.
- After participating in the myCME Case Clinic, 22% of learners said they would routinely implement suitable screening protocols for patients with symptomatic and asymptomatic AF “sometimes” or “rarely”; 8% said they would “never” do so.
- More than a quarter (28%) of myCME Case Clinic learners said they would not regularly employ evidence-based stroke-prevention protocols for patients with NVAF after participating in the activity.
- Meaningfully engaging patients in their own care can be challenging; although we achieved a sizable number of visits to the GetStrokeSmart site, patient survey participation was low.
Summary
This multicomponent CME/CE initiative was designed to create awareness of the magnitude of undiagnosed NVAF among clinicians and to provide education to facilitate identification and appropriate intervention. The Patient Education Program was utilized to increase awareness efforts at a grassroots level, close the loop between patient and HCP education and enhance the quality of physician-patient communication. Analysis of outcomes data showed significant improvements in learners’ knowledge, competence and practice relative to the activity learning objectives and, by extension, a positive impact on patient outcomes.
References
- Kirchhof P, Benussi S, Kotecha D, et al. 2016 ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS: The Task Force for the Management of Atrial Fibrillation of the European Society of Cardiology (ESC): developed with the special contribution of the European Heart Rhythm Association (EHRA) of the ESC endorsed by the European Stroke Organisation (ESO). Eur J Cardiothorac Surg. 2016;37:2893-2962.
- Moran PS, Flattery MJ, Teljeur C, et al. Effectiveness of systematic screening for the detection of atrial fibrillation. Cochrane Database Syst Rev. 2013;(4):CD009586.
- Furberg CD, Psaty BM, Manolio TA, et al. Prevalence of atrial fibrillation in elderly subjects (the Cardiovascular Health Study). Am J Cardiol. 1994;74:236-241.
- Savelieva I, Camm AC. Clinical relevance of silent atrial fibrillation: prevalence, prognosis, quality of life and management. J Interven Card Electrophys. 2000;4:369-382.
- Lin HJ, Wolf PA, Kelly-Hayes M, et al. Stroke severity in atrial fibrillation. The Framingham study. Stroke. 1996;27:1760-1764.
- Hart RG, Benavente O, McBride R, Pearce LA. Antithrombotic therapy to prevent stroke in patients with atrial fibrillation: a meta-analysis. Ann Intern Med. 1999;131:492-501.
- Camm AJ, Lip GY, De Caterina R, et al. Focused update of the ESC guidelines for the management of atrial fibrillation: an update of the 2010 ESC guidelines for the management of atrial fibrillation: developed with the special contribution of the European Heart Rhythm Association. Eur Heart J. 2012;33:2719-2747.
- Björck S, Palaszewski B, Friberg L, Bergfeldt L. Atrial fibrillation, stroke risk, and warfarin therapy revisited: a population-based study. Stroke. 2013;44:3103-3108.
- Nieuwlaat R, Olsson SB, Lip GY, et al. Guideline-adherent antithrombotic treatment is associated with improved outcomes compared with undertreatment in high-risk patients with atrial fibrillation: the Euro Heart Survey on Atrial Fibrillation. Am Heart J. 2007;153:1006-1012.