Clinical Context
Due to nonspecific symptoms and overlapping seasonality, primary and urgent care providers are particularly challenged to differentiate influenza (flu) infection from COVID-19. Because antiviral therapies must be administered within the first few days of infection, education was needed for frontline providers to improve differential diagnosis and management, particularly for patients at high risk of severe complications due to flu infection. To address this issue, Vindico Medical Education (Vindico), an accredited continuing education (CE) provider, partnered with American Family Care (AFC), a network of 500+ urgent/primary care practices, to deliver a comprehensive live webinar for primary and urgent care providers who manage patients presenting with flu-like symptoms.
Traditional assessments were used to quantify the impact of the education on knowledge and behaviors, while electronic medical record (EMR) queries were used to objectively measure changes in performance by AFC providers due to the education provided.
Educational Design
The goals of the program were to:
· Improve influenza symptom recognition to better utilize healthcare resources and identify patients with flu in a timely manner.
· Treat patients with confirmed influenza according to the latest evidence and recommendations.
· Utilize antiviral prophylaxis for patients who are at high risk of influenza infection.
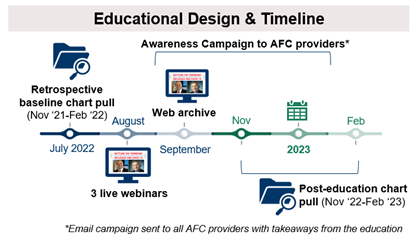
For the AFC providers, content was delivered as a 60-minute webinar, followed by a live, 15-minute Q&A session with faculty. To accommodate various time zones and schedules, the webinar was offered at three different times. The webinar was also archived online to increase provider reach. A robust awareness campaign was delivered to AFC providers to reinforce messaging within the network.
To achieve objective measures of behavior changes, baseline and post-education queries of the EMRs of patients seen at AFC clinics during the 2021–2022 (baseline) and 2022–2023 (post-education) influenza seasons was performed.
Results
One hundred thirty-five AFC providers participated in the education. Baseline knowledge was low for all topics but particularly related to the use of chemoprophylaxis for high-risk patients. Overall, there was an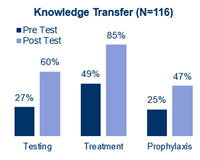 84% relative increase in knowledge from pre-test to post-test. Thirty days post-learning, 60% of the AFC survey respondents (N=13) had implemented changes into practice, including improved use of assays to differentiate influenza from COVID-19 and use of empiric treatment for high-risk patients. These findings are validated by the chart pull data. Of those who reported implementing practice changes, 77% reported improvements in patient health.
84% relative increase in knowledge from pre-test to post-test. Thirty days post-learning, 60% of the AFC survey respondents (N=13) had implemented changes into practice, including improved use of assays to differentiate influenza from COVID-19 and use of empiric treatment for high-risk patients. These findings are validated by the chart pull data. Of those who reported implementing practice changes, 77% reported improvements in patient health.
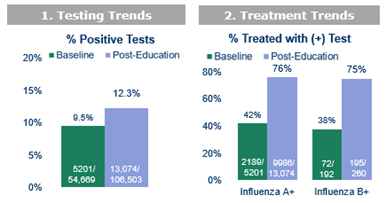
The use of EMR queries within the AFC network of providers allowed for the objective measure of the educational impact on influenza testing and treatment. Specific EMR queries were based on all patients with influenza tests ordered by the 135 participating AFC providers in the baseline (November 2021–February 2022) and post-activity (November 2022–February 2023) flu seasons. Parameter data are as follows: (1) influenza test result, (2) presence of asthma and/or diabetes and (3) antiviral prescription ordered (if any).
The results and clinical significance are summarized as follows:
1. Twenty-nine percent increase in positive influenza test rate from the baseline to post-education time period, indicating improved symptom recognition and the use of healthcare resources.
2. Increased rate of treatment of patients with confirmed influenza A or B in the post-education period (72% or 83% increase, respectively) compared with the baseline period, equating to 10,181 patients who received treatment proven to decrease hospitalization and mortality, among other benefits.
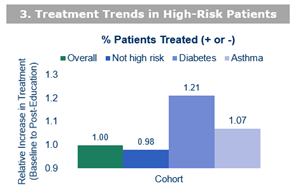
3. More than a two-fold increased rate of treatment or empiric treatment of high-risk patients, which aligns with the Centers for Disease Control and Prevention guideline recommendations for the management of patients with diabetes or asthma who present with flu-like symptoms. The relative increase in treatment of high-risk patients was greater for those with diabetes or asthma (21% or 7%, respectively) versus patients without risk factors. This equates to 681 more patients with diabetes and 737 more patients with asthma who received evidence-based treatment.
Discussion
Measurement of performance change in CE programs is often too subjective (e.g., self-reported surveys), time delayed (e.g., claims data) or costly (quality improvement initiatives). Using a closed-network design, Vindico provided education within the AFC network, and AFC was able to provide access to patient-level data to quantify the changes in testing and treatment from baseline to post-learning in a cost-effective manner. While traditional methods to assess knowledge, competence and behaviors were also implemented, the EMR query both validates the subjective measures of performance change and adds more details regarding the number of patients who directly benefited from this education and in what manner.
Importantly, this study illustrates the benefits of collaboration between medical education companies and health systems to deliver and assess the benefits of meaningful CE to a network of providers. Additional educational efforts between Vindico and AFC are ongoing. CE professionals seeking to elevate their outcomes assessments can seek similar partnerships with healthcare networks who may be looking to elevate their educational opportunities for HCPs within their network.
This educational initiative was supported through an educational grant from Genentech, a member of the Roche Group.
 Katie Robinson, PhD, CHCP, is the senior director, outcomes and analytics, for Vindico Medical Education.
Katie Robinson, PhD, CHCP, is the senior director, outcomes and analytics, for Vindico Medical Education.
 Jessica Higginbotham, PharmD, BCGP, BCCP, is the vice president of pharmacy services for American Family Care.
Jessica Higginbotham, PharmD, BCGP, BCCP, is the vice president of pharmacy services for American Family Care.