Effective communication and interpersonal skills are essential in healthcare, especially when delivering complex or sensitive information to patients. Research supports the benefits of simulation for skill development and patient safety. Simulation-based training has been shown to contribute significantly to building a culture of safety within healthcare organizations.1-2 Furthermore, simulation has proven to be an effective tool for both developing and assessing healthcare-related interpersonal skills, enhancing providers' competence in real-world settings.3
AI-driven tools such as virtual patient simulation platforms offer a new way to bridge training gaps. A recent study, conducted by a CME provider and Xuron, examined the impact of oncology-focused AI-guided simulation training among a cohort of clinicians, and the findings show that such simulation-based education is an effective and engaging learning format.
Research Overview
Clinicians in the study included a diverse group of healthcare professionals, including pharmacists, nurse, a nurse manager and a physician, all aged between 35 and 60 (n = 5). The clinicians were introduced to two video-based activities that were delivered as AI-driven simulations. The first video illustrated an HCP-AI patient interaction, while the second demonstrated AI-provided feedback on the healthcare provider’s performance, based on targeted simulation steps and learning objectives (LOs). Participants evaluated realism, engagement, usefulness and the relevance of AI-generated feedback.
Limitations
Several limitations must be considered when interpreting these results. The limited sample size constrains the generalizability of the findings. Additionally, participants viewed pre-recorded interactions rather than engaging in live simulations, which may have affected their perceptions of realism and interactivity. The study also lacked a control group, making it difficult to compare the AI-driven simulation's effectiveness against traditional training methods.
Course Description
In this course, learners tackle communication challenges in palliative and hospice care. The simulation features a 35-year-old patient with metastatic breast cancer who, after multiple chemotherapy regimens, shifts focus from curative treatments to palliative care. Learners first build foundational knowledge in palliative care and then actively implement this knowledge during the simulated conversation, refining their clinical communication skills with personalized, standardized, and actionable feedback and scoring (Likert scale 1-5). 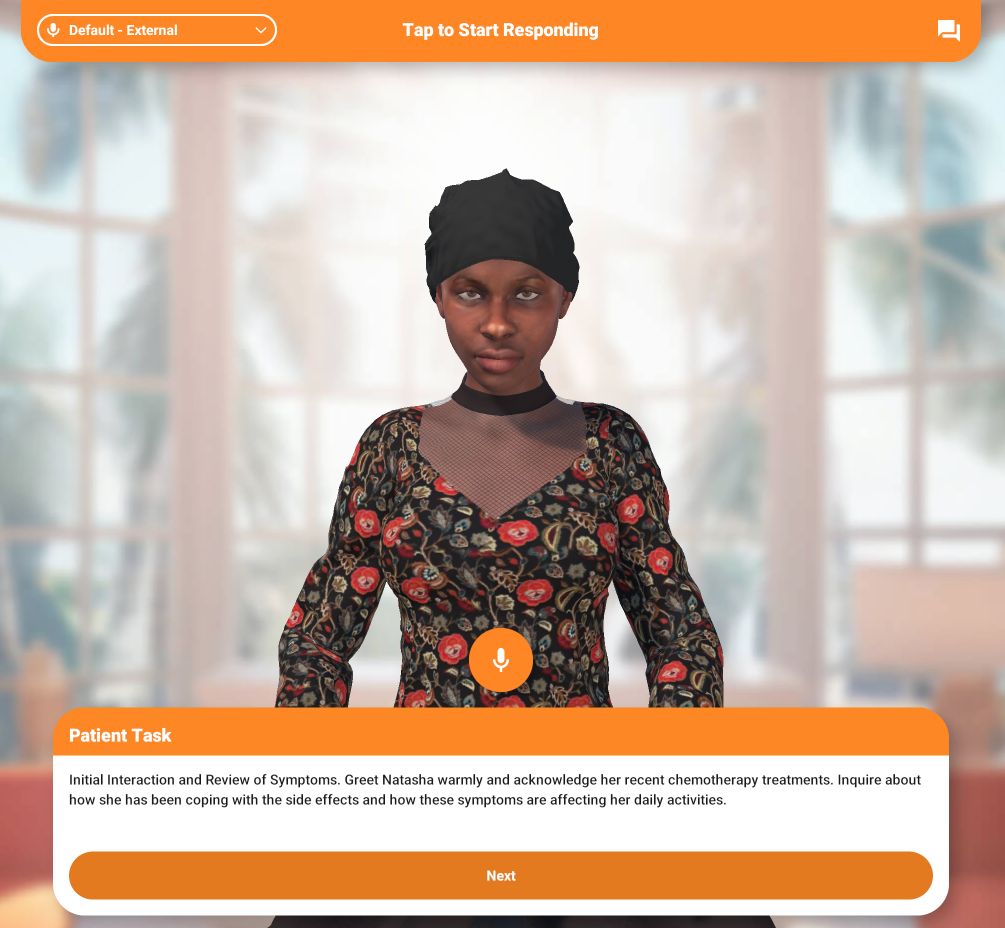
Key Findings
Realism: Participants generally found the AI patient interaction to be moderately realistic, rating it a 3.2 out of 5. Some participants felt the conversation flow was somewhat segmented and lacked the natural back-and-forth of real-life interactions.
Another mentioned, “Felt pretty real, especially the part where they were resisting after the HCP said that they had exhausted all treatment options. What the patient was saying felt very believable and understandable, and it also showed the emotional side as well.”
Engagement: Despite the critique on realism, the platform was rated as highly engaging, with particular note on the immersive nature of AI-driven simulation and a mean score of 4.4 out of 5. One participant commented, “This felt more engaging. I prefer this over the regular activities.”
Perceived Value: The perceived usefulness of the simulation platform was evaluated as an average of 4.3 out of 5, reflecting its potential as a valuable training tool, especially for professionals at different stages in their careers.
As one participant noted, “Watching this video gave me [an] opportunity to think about situations I’ve been in myself. I don’t usually get to see other providers having these kinds of conversations with patients, so even watching the video of the conversation was interesting.”
A nurse manager participant noted: “I really like this. [In] [m]y position right now as a nurse manager, I have some nurses who went to school during COVID. They did a lot of online stuff, and they are just so uncomfortable talking with patients or trying to explain things to the patient or their family. I think this would be a great tool to expose these guys just to have them be more comfortable when interacting with a real patient.”
Relevance of AI-generated Feedback: A well-scored feature of the simulation activity was the AI-generated feedback of learner’s skills. One user highlighted, “The feedback from the second part where AI is giving the feedback, I really like that. If I had to rate that by itself, I'd give it a five because I think it's really good.”
Another participant noted, “I like that it gave pointers as to how to lead the conversation and wording things in laymen’s terms,” comparing it to the valuable insights one might receive from an in-person mentor.
Interest in Future Use: Clinicians expressed a strong interest in using AI-driven simulations for learning in the future, with an average score of 4.8 out of 5, underscoring a significant interest in this interactive learning model. One learner said, “I definitely tend to lean more toward the interactive than just reading an article and answering questions.”
Trust in AI-powered Tools: While trust in AI-powered simulation was high at a 4 out of 5 average score, clinician learners expressed a desire for continued exposure to further build confidence in AI-driven education. One user stated, “I would imagine that the tool has multiple sources, it’s not like it’s just drawing from Wikipedia.”
Another remarked, “AI is good until it gets into details, then I don’t know how much they would be able to help. I would want to try the tool and see for myself.”
Discussion
The pilot study highlights the potential of AI-driven simulation in CME for practicing challenging conversations in palliative and hospice care. In this evaluation, five healthcare clinicians reviewed a video demonstration that showcased both a simulated patient interaction — featuring a 35-year-old patient transitioning from curative to palliative care — and the system’s AI-generated feedback process. Participants rated the demonstration with a realism score of 3.2 out of 5, while engagement, perceived value, and interest in future use scored 4.4, 4.3, and 4.8, respectively. Although these findings are based on a pre-recorded demonstration rather than direct interaction with the platform, they effectively illustrate the system’s potential to enhance communication competencies in sensitive clinical scenarios.
The evaluators particularly appreciated the personalized feedback provided at the end of the simulation. Central to this approach is the AI component, developed using detailed evaluation criteria and rubrics for each simulation step. Trained on numerous examples of scoring and best practices for delivering effective feedback, the AI generates personalized, actionable evaluations — without human-in-the-loop review — that closely mirror expert human assessments. Ongoing validation studies comparing AI-generated feedback with human evaluations are currently underway to better establish the credibility of this method.
Recent research supports the integration of AI into simulations to enhance communication skills among healthcare professionals. These AI-driven simulations offer realistic scenarios that allow practitioners to practice and refine their interpersonal skills in a safe environment, thereby improving patient safety and care quality. Studies have demonstrated that such AI-driven simulations not only bolster communication competencies but also provide measurable evidence of learners' readiness for clinical practice. By immersing healthcare providers in authentic patient interactions, these tools facilitate the development of essential communication skills, which are crucial for effective patient care and collaboration within healthcare teams.4-7
Conclusion
AI-powered virtual simulation education demonstrates significant potential as an engaging and valuable tool for enhancing healthcare providers' interpersonal and communication skills. The findings from this research suggest that such AI-driven simulations could serve as effective alternatives or supplements to traditional CME activities. Nonetheless, the study's limitations highlight the need for further research. Future studies should aim to validate these findings across larger and more diverse populations and assess effectiveness in live, interactive settings to fully ascertain its role in healthcare education.
Acknowledgement: Many thanks to Caroline O. Pardo, PhD, CHCP, FACEHP, for her guidance on interpretation of the research results and implications to practice.
References
- Motola I, Devine LA, Chung HS, Sullivan JE, Issenberg SB. Simulation in healthcare education: A best evidence practical guide. AMEE Guide No. 82. Med Teach. 2013;35(10). https://doi.org/10.3109/0142159X.2013.818632
- McGaghie WC, Issenberg SB, Petrusa ER, Scalese RJ. A critical review of simulation-based medical education research: 2003–2009. Med Educ. 2010;44(1):50-63. https://doi.org/10.1111/j.1365-2923.2009.03547.x
- Lane C, Rollnick S. The use of simulated patients and role-play in communication skills training: A review of the literature to August 2005. Patient Educ Couns. 2007;67(1-2):13-20. https://doi.org/10.1016/j.pec.2007.02.011
- Anthamatten A, Holt JE. Integrating artificial intelligence into virtual simulations to develop entrustable professional activities. J Nurse Pract. 2024;20(9):105192. https://doi.org/10.1016/j.nurpra.2024.105192
- Cho MK, Kim MY. The effect of virtual reality simulation on nursing students’ communication skills: A systematic review and meta-analysis. Front Psychiatry. 2024;15:1351123. https://doi.org/10.3389/fpsyt.2024.1351123
- Farina CL, Moreno J, Schneidereith T. Using simulation to improve communication skills. Nurs Clin North Am. 2024;59(3):437-448. https://doi.org/10.1016/j.cnur.2024.02.007
- Turkelson C, Yorke AM, Keiser M, Smith L, Gilbert GE. Promoting interprofessional communication with virtual simulation and deliberate practice. Clin Simul Nurs. 2020;46:30-39. https://doi.org/10.1016/j.ecns.2020.03.008

Boris Rozenfeld, MD, has been immersed in medical education for over ten years, with expertise in adaptive learning technology, generative AI and innovative training design. Rozenfeld currently serves as the Medical Education Director at Xuron, where he develops AI-powered conversational simulations to teach and assess interpersonal, communication and clinical reasoning skills.

Ian Nott is the CEO of Xuron, where he leads a cross-disciplinary team revolutionizing medical training through AI-powered virtual human simulations. With nearly a decade of experience in spatial computing, and building complex software companies, his work focuses on empowering HCPs with advanced training tools for complex clinical scenarios and patient communication.