By Esther Nyarko, PharmD, and the Alliance Research Committee: Andrew D. Bowser ELS, CHCP; Allison Gardner PhD, CHCP; Alexandra Howson PhD, CHCP (Chair); Carla Jones MSN RN-BC; Leanne Perry Ed.D., MSN, RN, NPD-BC; Lisa M. Shook MA, MCHES
Introduction
Since the 1999 publication of the Institute of Medicine’s (IOM) investigation into the pervasiveness of medical error,1 governing and regulatory bodies have increasingly emphasized the importance of team-based healthcare delivery as a key strategy to promote patient safety. Healthcare teams are vital players in establishing a culture of safety and implementing viable solutions to address medical errors.
In turn, interprofessional education (Figure 1) has emerged as a foundation to support the development of competencies that enable health professionals to do the following:
- Provide patient-centered care
- Apply quality improvement
- Employ evidence-based practice
- Utilize informatics
- Work in interdisciplinary teams
Figure 1. Defining Interprofessional Education
- Interprofessional Education (IPE): When students from two or more professions learn with, from and about each other to enable effective collaboration and improve health outcomes.2
- Interprofessional Collaborative Practice (IPCP): When multiple health workers from different professional backgrounds work together with patients, families, careers and communities to deliver the highest quality of care.3
- Interprofessional Continuing Education (IPCE): When members from two or more professions learn with, from and about each other to enable effective collaboration and improve health outcomes.2
Joint Accreditation for Interprofessional Continuing Education promotes IPCE and offers organizations simultaneous accreditation for continuing education across a range of disciplines. This organization provides guidance and tools on how to effectively design education that changes the skills/strategy, performance and/or outcomes of the healthcare team and has outlined the following key characteristics of a successful IPCE program:3
- Supportive leadership
- Strong relationships among key stakeholders
- Purposeful communication
- Teamwork
|
The Value of Interprofessional Continuing Education
Interprofessional continuing education (IPCE) can be highly effective. For instance, a 2020 Joint Accreditation Leadership Summit report on “The Transformative Value of IPCE” highlights the impact of teams during the COVID pandemic.3 Despite many challenges, healthcare professionals were able to increase engagement across professions and demonstrate the value of IPCE within their organizations. The pandemic reinforced the importance of open communication not only within their respective practice settings, but across healthcare disciplines and all levels of government. To maintain a patient-centered focus, the healthcare team needed to effectively collaborate to reduce silos and personal or professional gain and obtain needed resources to combat COVID-19. Educators saw the opportunity of using IPCE as a platform to address important topics such as time management, communication, diversity, healthcare disparities, clinician burnout and resiliency.
However, despite the appeal of IPCE, its implementation can be challenging. Barriers to implementation that have been reported in the literature include territorial behaviors among professions; stereotyping of professions, expertise and professional abilities; lack of time; and lack of physician advocates and/or faculty who see the true value of IPCE.3
In order to learn how Alliance members are addressing IPCE in their own organizations and to identify barriers to implementing IPCE, the Alliance Research Committee fielded a survey to Alliance members in July 2021.
Alliance Survey Findings
The 93 survey respondents were distributed across the following sections: hospitals and health systems (27%), medical education companies (22%) and medical specialty societies (17%). Medical schools, professionals with education expertise, resources and services, Industry Alliance for CE and state medical societies comprised the remaining 31%.
Joint Accreditation
Joint Accreditation for IPCE is one pathway to provide IPCE. To qualify for Joint Accreditation, providers should ensure that at least 25% of continuing education activities are interprofessional. Providers need to show an integrated planning process that includes members of the two or more health professions which is reflective of their educational target audience. A majority (62%) of respondents indicated that they offer IPCE education in their organizations, while 14% indicated they were thinking about it and 24% of respondents indicated they are not pursuing IPCE in their organizations at this time.
Over one quarter (28%) of respondents have been offering IPCS for more than eight years; 46% have been offering IPCE education for one–eight years; and 5% have been offering IPCS for less than one year. Over one quarter (27%) of respondents offer IPCE through their organization’s Joint Accreditation status and 31% offer IPCE through multiple accreditations.
Team Related Competencies
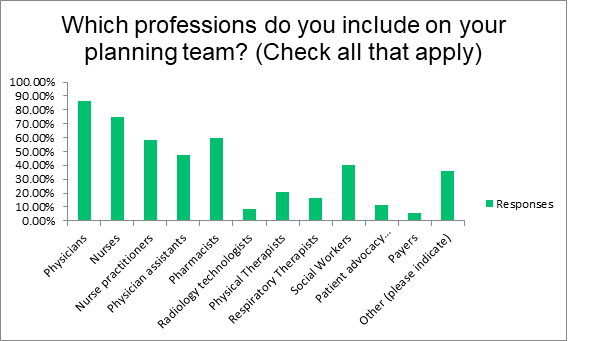
Team-related competencies enable members to collaborate, cooperate and communicate with each other to better integrate planning decisions that improve patient care. The goal of this communication, in addition to ensuring improved interpersonal interaction, is to enable members to get a better understanding of the roles of the members of the team, to better address the needs of the patients and their families. Effective IPCE planning requires inclusion on the planning team of health professionals that represent the target audience for whom the education is relevant. Survey respondents reported that they include various health professionals on their planning teams including physicians (86%), nurses (75%), pharmacists (60%) and nurse practitioners (58%). Other members cited include physician assistants, social workers, dosimetrists, physicists, researchers, dieticians, radiologists, patients, chaplains, medical assistants, athletic trainers and diabetes educators (Figure 2).
Figure 2. Professions Included in IPCE Planning Teams
Teamwork (69%), roles and responsibility (50%) and communication (54%) were the team-related competencies that respondents most reported. Value and ethics (15%) and “other” competencies (21%) were reported less frequently.
Barriers to IPCE Planning and Delivery
While a minority (11%) of respondents did not report any barriers to IPCE within their institutions, a majority (28%) cited “planner buy-in” as the biggest challenge in developing IPCE. Other barriers included financial support (11%), communication and administrative challenges (8.33%) and learner buy-in (5%). Responses to an open-ended question about barriers identified additional operational and categorical challenges such as:
- Meeting the filing deadlines for accreditation
- Lack of guidance from accrediting societies as to what constitutes IPCE
- Differences in levels of stakeholder buy-in
- Using evaluation and data insights as a platform for behavior change
Conclusion
IPCE has made inroads in patient management, but medical errors continue to be a public health concern in 2021 and remain a leading cause of death in the United States.4 Therefore, team-based care delivery is more important than ever to promote patient safety, and IPCE is a critical intervention to support team-based care. Survey findings reveal persistent challenges in the planning and implementation of IPCE, especially in relation to the relatively limited range of personnel involved in planning and point to a window of opportunity to further engage Alliance members in the value of team-based learning. The Research Committee plans to conduct focus groups with Alliance members to further explore these findings.
References
- Kohn L T, Corrigan J M, Donaldson MS (Institute of Medicine) To err is human: building a safer health system. Washington, DC: National Academy Press, 2000
- World Health Organization (WHO). Framework for Action on Interprofessional Education and Collaborative Practice. Geneva, Switzerland: World Health Organization. 2010. WHO Publication: WHO/HRH/HPN/10.3. Available at: www.who.int/hrh/resources/framework_action/en/index.html. Accessed October 2021
- Joint Accreditation for Interprofessional Continuing Education. Available at: www.jointaccreditation.org. Accessed October 2021
- Ahmad F, Anderson R N, The Leading Causes of Death in the US for 2020, JAMA 2021;325 (18)1829-1830