Introduction
Outcomes in CE have traditionally relied on pre- and post-education assessment of knowledge, competence and/or performance. While an emphasis on measurable outcomes has driven the evolution of CE toward more evidence-based and impactful learning, these types of measures are heavily reliant on sound question writing and learner self-report, leaving a lot of unanswered questions regarding drivers for learning and/or clinical decision-making. Incorporating questions that encourage the learner to reflect on their underlying attitudes or perceptions toward a particular topic is an easy way to draw meaningful information that can be used to provide a deeper understanding of the data collected from traditional measures and refine the development of future education. In the same vein, these types of questions can be integrated into models for follow-up assessments to show impact of education on attitudes and perceptions overtime.
Results
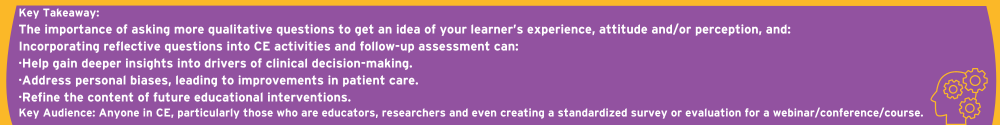
A portion of the agenda in the comprehensive CE activity, “Obesity Forum”, included an interactive segment in which attendees were challenged to rate their agreement regarding several common misconceptions about obesity and use of obesity medications (OMs). Five-point Likert rating scales were used. To assess changes in biases overtime, 30 days later, completers of the program were sent a follow-up CE activity featuring the same questions. As shown in Figure 1, at follow-up, primary care providers (PCPs) were 25% more likely to agree that obesity is a disease and 28% more likely to disagree that it is a lifestyle decision. They also have increased perception that OMs are safe, can help achieve weight loss goals, and must be used in the long term. Of note, 74% report being more aware of their own personal biases toward the management of patients with obesity, with 26% reporting no change.
Figure 1: PCPs show improved attitudes towards obesity as a disease and OM use
Importantly, the changes in these personal biases contributed to increased comfortability in using OMs, as evidenced by a 19% increase in comfort. This also translated into 58% of PCPs noting that their use of OMs increased since participating in this sequential learning model (Figure 2).
Figure 2: PCPs show increased comfort in using OMs and increased use of OMs.
Discussion
This educational model unequivocally demonstrates that CE can be used to address and assess personal biases regarding the management of patients with obesity. It can also be used to help identify attitudes that may be hindering certain practices. For instance, shown here, during the initial CE, most PCPs were neutral regarding topics related to obesity as a disease versus a lifestyle decision, though most agreed that OMs can help achieve weight loss goals. At follow-up, there was an increase in those who viewed obesity as a disease. This, coupled with a more positive perception of OMs at follow-up, contributed to increase comfortability in OM use as well as increased use of OMs.
While the data presented here was for an educational program related to the management of patients with obesity, the following key points are highlighted for those who want to incorporate a similar approach in their own education:
- While not required, Likert rating scales are a good method for question writing, as changes can be easily quantified and compared at various points in time.
- If looking to compare changes in attitudes, at least some, if not all, questions should be phrased the same way across assessments.
- Questions can be integrated into the learning itself, as opposed to just in a pre-test or post-education assessment. This not only boosts engagement with the content, but it also reduces question fatigue for the learner.
- Faculty insights and/or pre-planning data collected from clinicians can help in crafting questions.
- This approach can be easily adapted to any live or web-based format and most therapeutic areas.
Conclusion
This study highlights the value of incorporating reflective questions into CE programs to assess and address personal biases and attitudes in clinical practice. In using this approach, educators can gain deeper insights into the underlying drivers of clinical decision-making and refine future educational interventions accordingly. This model provides a scalable and adaptable framework for enhancing the impact of CE across various therapeutic areas, ultimately leading to more effective and empathetic patient care.
Katie Robinson, Ph.D., CHCP, is the vice president, instructional design and analytics, for Vindico Medical Education.