Continued HIV treatment innovation has delivered a succession of ever-improving antiretroviral therapy (ART) options for people with HIV with optimized efficacy, safety and tolerability profiles.1 Healthcare professionals (HCPs) have a wealth of options from which to choose when selecting initial regimens, when modifying ART in virologically suppressed individuals and when constructing a new regimen for people experiencing virologic failure. In each of these settings, guidelines stress the importance of individualized regimen selection, taking account of treatment-related and patient-related factors ranging from treatment history to comorbidities and comedications.2,3 Despite this, gap analyses from Clinical Care Options (CCO) demonstrate that many HCPs struggle to make ART choices that align with the evidence-based decisions of experts. It is reasonable to expect that nonspecialist HCPs may be the most in need of tools that can help them make optimal decisions.4,5
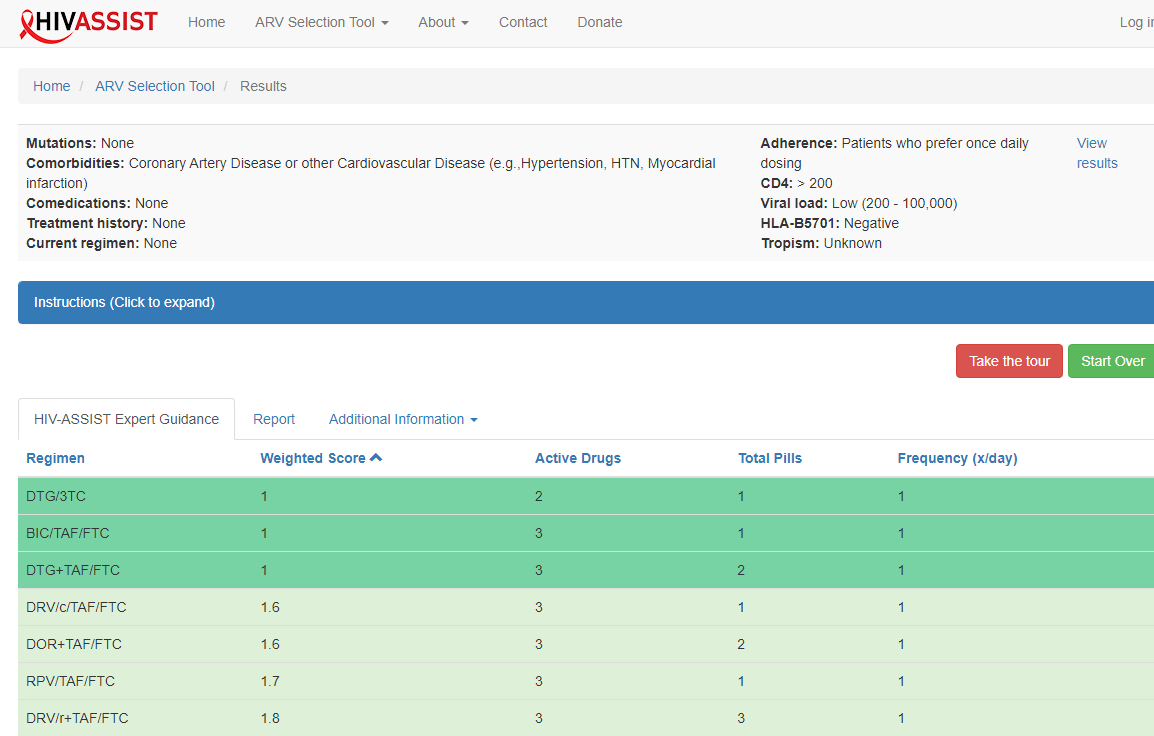
HIV-ASSIST is a validated clinical decision support tool created by HCPs at Johns Hopkins University to inform clinical decision-making for ART selection for people with HIV.6-8 It uses an expert-informed algorithm to provide ranked ART options for HCPs to consider in specific patient scenarios (see Figure 1). Patient- and viral-specific factors such as HIV viral load, CD4 cell count, viral mutations, adherence factors, comorbidities, comedications, ART history and current ART regimen are entered by users and evaluated by the tool’s algorithms to prioritize regimens most likely to be effective and well-tolerated.
Figure 1. HIV-ASSIST example output.
To maximize the use of this tool to improve HIV management, CCO and HIV-ASSIST collaborated on a series of educational activities. The goal of this collaborative educational program was to improve the competence and confidence of primary care providers and other nonspecialists in making evidence-based treatment decisions by increasing awareness and use of HIV-ASSIST.
Educational Design
The educational program consisted of multiple activities designed and presented with relevant partners to reach two target audiences with unique educational needs: community-based HIV-treating generalists and advanced practice providers (nurse practitioners [NPs] and physician associates [PAs]).
To reach and educate the first audience, nonspecialist HCPs and other community-based HIV-treating generalists, CCO and HealthHIV (a national nonprofit with extended reach to community-based HIV-treating generalists) developed a CME/CPE/CE-certified live webinar with an enduring online version and downloadable slides. The curriculum was designed to introduce HIV-ASSIST to this HCP audience, who may not have encountered it to date, and to support them in integrating use of the tool into their patient care to increase confidence with making ART decisions in practice. The activities began with demonstrations of how to use the tool, including both the online version and the mobile application, when making evidence-based ART decisions, and then applied the tool to patient case study scenarios focused on applicability in primary care. Live webinars were chosen as an educational format to give learners the opportunity to pose questions to experts in real time.
To reach and educate the second audience, advanced practice providers, CCO worked with NP and PA faculty to repurpose the live webinar as a live CME/CE-certified workshop with downloadable slides focused on applicability in primary care. This tailored workshop was presented by NP faculty at three different dates and times at the Annual Primary Care Series hosted by Practicing Clinicians Exchange (PCE), a CME provider that reaches an expansive network of NPs and PAs, many of whom work in primary care.
For each unique audience, short blog posts (termed “ClinicalThoughts”) and podcasts were developed outlining the use of HIV-ASSIST in making ART choices in patient scenarios typical of those seen frequently by nonspecialist providers. These microlearning formats were chosen to provide short examples that busy HCPs could easily find time to review. The ClinicalThoughts, in particular, were available as “push” education, delivered directly to learners’ email inboxes, removing barriers or inconvenience associated with reading web-based content.
Audience reach was measured. Outcomes measurements of awareness of the tool, competence in its use, and intention to use it in future practice were evaluated using pre/post and polling questions throughout the live events. In addition, metrics provided from HIV-ASSIST on usage were evaluated.
Continuing education credit was provided by CCO, with the support of independent educational grants from Gilead Sciences, Inc., and ViiV Healthcare.
Program Outcomes
Learners
The education successfully reached the target audiences of nonexpert HIV treaters. The live activities alone reached 1,624 learners: 590 learners at live CCO events targeted to US nonspecialists (almost half of whom identified as non-HIV/ID specialists) and 1,034 learners at live PCE events targeted to NPs/PAs (almost all of whom identified as non-HIV/ID specialists).
In addition to the live events, 10,424 learners participated in associated online activities targeted to primary care providers, including on-demand webcasts and downloadable slidesets from the live events to extend the reach, plus podcasts and ClinicalThoughts that reinforced the learning with case examples. This resulted in 13,767 online cumulative learnings across these primary care-focused activities from Feb. 14, 2023, to Dec. 12, 2023.
Outcomes Results
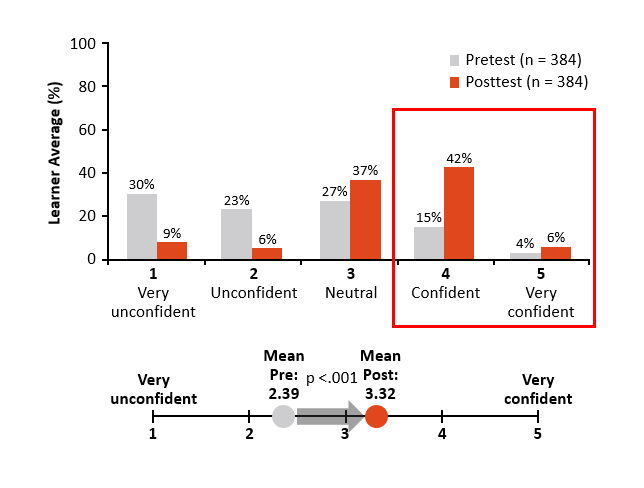
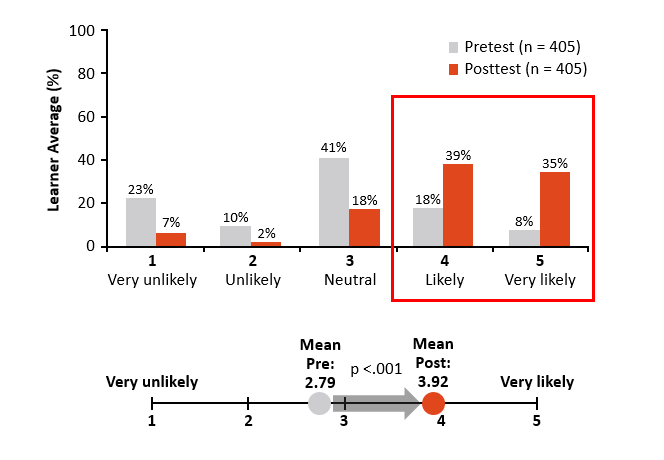
Beyond building awareness about the tool among the target audiences, this tailored approach to education had a significant impact on each set of learners, as demonstrated by pre- and post-education assessments (see Figure 2).
Figure 2. Effect of education on learners’ (a) confidence in managing HIV and (b) likelihood to use HIV-ASSIST.
Live Webinar and Enduring Webcast Combined: HIV-ASSIST for Primary Care Providers
- Outcomes Question 1: Confidence in Managing HIV
Pre-education assessment: Currently, how confident are you in managing HIV? (n = 384)
Post-education assessment: After participating in this activity and knowing that HIV-ASSIST is available to you, how confident are you in managing HIV? (n = 384)
- Outcomes Question 2: Likelihood of Using HIV-ASSIST
Pre-education assessment: Currently, how likely are you to use HIV-ASSIST as a resource for initiating or changing ART in patients with HIV? (n = 405)
Post-education assessment: After participating in this activity, how likely are you to use HIV-ASSIST as a resource for initiating or changing ART in patients with HIV? (n = 405)
After the education, the target audiences that included nonspecialist learners and NP/PA learners indicated that they were more confident in making HIV treatment decisions knowing that HIV-ASSIST is available: The proportion self-reporting as “confident” or “very confident” was only 17% before the education but increased to 49% after the education.
Moreover, they were more likely to use HIV-ASSIST as a resource for initiating or changing ART in people with HIV: The proportion self-reporting as “likely” or “very likely” to use HIV-ASSIST was only 24% before the education but increased to 73% after the education. One live participant asked the faculty if they had “experience with using [HIV-ASSIST] in shared fashion during patient visits.” This led to a discussion of the possibility for the HIV-ASSIST tool to be used during patient visits to facilitate shared decision-making.
Impact on Practice
In addition to measuring intention to use the tool when making treatment decisions to improve patient care, we also directly measured actual use of the tool. HIV-ASSIST's analysis of the use of their tool suggests that these educational activities led to increased tool usage, measured both as increases in the number of cases entered (which increased 55% year over year during the same months of the education) and increases in the number of unique users. Although the tool may be used anonymously, available site data suggest a near doubling (1.8 times) of unique users of the tool during the period of the educational activities compared with prior years. Registered users to the site, which provides added services including the ability to save cases, also have proliferated, such that 44% of all new accounts created (since 2016) occurred during the period of the current educational activities. Although the proportion of users accessing HIV-ASSIST on smartphones remains low, there was a 10-fold increase in tool usage from mobile devices compared with the previous year.
Future Educational Needs
The live events also gave us insight into the types of cases where a tool for clinical decision-making in HIV care is needed, which revealed educational gaps for these audiences. Questions from the audience indicated that more complex and diverse patient case scenarios should be included in future education and that cases with drug-drug interactions, comorbidities and coinfections would be most useful, in addition to more case examples of rapid initiation, or same-day, ART with different baseline patient characteristics. Specific questions asked by participants included:
- “How would you use this in a rapid start scenario?”
- “How many drug interactions does the algorithm take?”
- “Does HIV-ASSIST provide accurate regimens for patients on meds for tuberculosis?”
- “Is age at initiation of therapy input to account for potential comorbidities?”
- “Can you share when to prescribe the long-acting shots?”
- “Is there anything that takes into consideration possible polysubstance use?”
- “What is the cutoff viral load to switch from a 3 to 2 drug regimen?”
- “What nutritional indications do patients with HIV have, and do any of the HIV meds interact with foods?”
- “Client is treatment experienced with protease inhibitor resistance: They now test positive for COVID. Is the current treatment an option?”
- “Can the tool also be used for pre-exposure [or postexposure] prophylaxis selection?”
- “Is there a similar resource or a section within the tool that helps guide other screenings/recommendations for preventive care for patients with HIV (e.g., CMV screening, etc.)?”
Conclusions
The educational collaboration between CCO and HIV-ASSIST, in partnership with HealthHIV and PCE, was successful in demonstrating the value of a tool to increase the confidence of primary care and nonspecialist providers in clinical decision-making when initiating and changing ART for people with HIV. HIV-treating generalists and advanced practice provider learners indicated that they were more aware of the tool, more confident in using it and more likely to incorporate it into their practices to improve HIV management. Following the education, actual use of the tool increased, as measured by growth in number of cases entered and number of unique users, indicating a positive impact on practice and benefit to patients in the real world. Questions posed by participants in the educational activities provided insight on future education needed to further familiarize nonspecialist HCP audiences with the HIV-ASSIST tool and increase confidence and competence in managing ART in more complex clinical scenarios.
References
- National Institutes of Health. FDA-approved HIV medicines. hivinfo.nih.gov/understanding-hiv/fact-sheets/fda-approved-hiv-medicines. Accessed April 3, 2024.
- US Department of Health and Human Services. Panel on Antiretroviral Guidelines for Adults and Adolescents. Guidelines for the use of antiretroviral agents in HIV-1-infected adults and adolescents. clinicalinfo.hiv.gov/en/guidelines/hiv-clinical-guidelines-adult-and-adolescent-arv. Accessed April 3, 2024.
- Gandhi RT, Bedimo R, Hoy JF, et al. Antiretroviral drugs for treatment and prevention of HIV infection in adults: 2022 recommendations of the International Antiviral Society-USA Panel. JAMA. 2023;329:63-84.
- Clinical Care Options. Data on file. HIV Survey. 2021.
- Gilman B, Bouchery E, Hogan P, et al. The HIV clinician workforce in the United States: supply and demand projections from 2010 to 2015. American Academy of HIV Medicine. HIV Specialist. August 2016;8:2-9.
- Maddali MV, Mehtani NJ, Converse C, et al. Development and validation of HIV-ASSIST, an online, educational, clinical decision support tool to guide patient-centered ARV regimen selection. J Acquir Immune Defic Syndr. 2019;82:188-194.
- Ramirez JA, Maddali MV, Budak JZ, et al. Evaluating the concordance of clinician antiretroviral prescribing practices and HIV-ASSIST, an online clinical decision support tool. J Gen Intern Med. 2020;35:1498-1503.
- Ramirez JA, Maddali MV, Nematollahi S, et al. New strategies in clinical guideline delivery: randomized trial of online, interactive decision support versus guidelines for human immunodeficiency virus treatment selection by trainees. Clin Infect Dis. 2021;72:1608-1614.
This program was supported by independent educational grants from Gilead Sciences, Inc. and ViiV Healthcare.

Jessica Adams, PharmD, AAHIVE, has experience in clinical practice, education and research and is passionate about optimizing treatment for people living with HIV and other infectious diseases. She received her Doctor of Pharmacy degree from Albany College of Pharmacy and Health Sciences, completed residency at Henry Ford Hospital in Detroit Michigan, and an academic fellowship in HIV Pharmacology at the University of North Carolina at Chapel Hill.

Zachary Schwartz, MSc, ELS, has worked in the field of CME and medical communication since 1997. He has collaborated closely with key opinion leaders in the development of educational programming across many therapeutic areas, including infectious diseases, cardiology, immunology, neurology, oncology and primary care. Zachary is certified by the Board of Editors in the Life Sciences and earned his MSc in neurology and neurosurgery from McGill University in Montreal.
 Jenny Schulz, Ph.D., has nearly 20 years of experience in continuing professional development, with expertise in HIV, viral hepatitis and other infectious diseases. In her CPD work, Jenny has led teams working on educational design and on program implementation. She excels in building relationships with thought leaders, forging strategic partnerships that elevate program design, and in utilizing innovative models that meet the needs of today’s healthcare professionals. Jenny is committed to improving patient lives and approaches her work with this central focus. She has coauthored more than a dozen presentations or publications in infectious disease CPD, including abstracts at IDWeek, The Liver Meeting, and the European Association of the Liver, and publication in the Journal of Viral Hepatitis. Jenny received her B.S. in biology from Drake University in Des Moines, Iowa, and her Ph.D. from the Division of Biological and Biomedical Sciences at Emory University in Atlanta.
Jenny Schulz, Ph.D., has nearly 20 years of experience in continuing professional development, with expertise in HIV, viral hepatitis and other infectious diseases. In her CPD work, Jenny has led teams working on educational design and on program implementation. She excels in building relationships with thought leaders, forging strategic partnerships that elevate program design, and in utilizing innovative models that meet the needs of today’s healthcare professionals. Jenny is committed to improving patient lives and approaches her work with this central focus. She has coauthored more than a dozen presentations or publications in infectious disease CPD, including abstracts at IDWeek, The Liver Meeting, and the European Association of the Liver, and publication in the Journal of Viral Hepatitis. Jenny received her B.S. in biology from Drake University in Des Moines, Iowa, and her Ph.D. from the Division of Biological and Biomedical Sciences at Emory University in Atlanta.
 Maunank Shah, M.D., is a professor in the Division of Infectious Diseases at Johns Hopkins School of Medicine, and Department of Epidemiology in the Johns Hopkins School of Public Health. He is medical director of the Baltimore Tuberculosis Program and is president of the U.S. National Society of Tuberculosis Clinicians. Dr. Shah’s research involves evaluating and implementing novel HIV and tuberculosis (TB) intervention strategies in both low and high-incidence settings. He has evaluated new TB diagnostic technologies and assessed the cost-effectiveness of emerging strategies for HIV and TB care in multiple locations. He led the evidence review for the WHO Guideline Development Group for usage of Urinary LAM for diagnosis of TB and is formerly the Maryland site PI for the CDC TB Epidemiologic Studies Consortium. He is co-inventor of the electronic directly observed therapy platform used in more than 500 health departments in the U.S. (www.Scene.com), and has led development and implementation of an online electronic TB consultation platform for the Northeast Regional CDC funded TB Center of Excellence (Rutgers.IDCrowd.Org). He is the co-inventor of HIV-ASSIST (www.hivassist.com), a validated, easy-to-use online and mobile ARV decision support tool. Dr. Shah serves as the deputy editor for the primary clinical journal of the Infectious Diseases Society of America—Clinical Infectious Diseases (CID).
Maunank Shah, M.D., is a professor in the Division of Infectious Diseases at Johns Hopkins School of Medicine, and Department of Epidemiology in the Johns Hopkins School of Public Health. He is medical director of the Baltimore Tuberculosis Program and is president of the U.S. National Society of Tuberculosis Clinicians. Dr. Shah’s research involves evaluating and implementing novel HIV and tuberculosis (TB) intervention strategies in both low and high-incidence settings. He has evaluated new TB diagnostic technologies and assessed the cost-effectiveness of emerging strategies for HIV and TB care in multiple locations. He led the evidence review for the WHO Guideline Development Group for usage of Urinary LAM for diagnosis of TB and is formerly the Maryland site PI for the CDC TB Epidemiologic Studies Consortium. He is co-inventor of the electronic directly observed therapy platform used in more than 500 health departments in the U.S. (www.Scene.com), and has led development and implementation of an online electronic TB consultation platform for the Northeast Regional CDC funded TB Center of Excellence (Rutgers.IDCrowd.Org). He is the co-inventor of HIV-ASSIST (www.hivassist.com), a validated, easy-to-use online and mobile ARV decision support tool. Dr. Shah serves as the deputy editor for the primary clinical journal of the Infectious Diseases Society of America—Clinical Infectious Diseases (CID).
Author Affiliations
- Clinical Care Options, Clinical Education Alliance, Reston, Virigina
- HIV-ASSIST, Inc
- Johns Hopkins University, Baltimore, Maryland