
We certainly do use our share of acronyms within the field of continuing professional development. We utilize them to describe the field (CPD, IPCE, CME, MOC, PRA); our practices (COI, LOA, etc); accrediting/oversight organizations (AMA, ACCME, ACGME, AHA, ACPE, ANCC, AAMC, CMSS, FSMB, NBME, etc); and specialty boards (ABMS, AAAAI, AAFP, ABIM, ABS, ABP, etc). And that is just for starters.
You get the idea. The field reflects a veritable acronym soup that may even rival the extensive ingredient lists utilized by those who work in technology. This new vocabulary can be overwhelming for someone new to the field of CPD, as at times it may seem their peers are speaking another language.
Dependent upon the level of business or strategic planning experience the interpreter brings to their role, their perception of various terms may be quite varied. Sometimes the public narrative and/or individual’s experience level and/or historical perspective can add confusion and result in an incomplete or distorted view.
For the purpose of this article, let’s focus on one term that has frequently made its way into the headlines, D-E-I (Diversity, Equity, and Inclusion). DEI programs have become one of the most polarizing topics in the United States, and the term itself is now at the center of heated debates about fairness, merit, and identity.
Many organizations consider DEI policies, practices, and programs to be core to their ability to attract, develop, and retain talent. Others may express concern that these efforts may be interpreted as quotas, giving unfair advantage to some groups over others.
Specific to the CPD field, the Alliance for Continuing Education in the Health Professions (ACEHP) outlines its formal commitment to DEI (Alliance for Continuing Education in the Health Professions > Archive Pages > Resources > DEI Resources). Its DEI policy lists core principles which include promoting equitable opportunities and valuing diversity across professions and practice settings. It details actions like providing education and amplifying underrepresented voices. Similarly, the Accreditation Council for Continuing Medical Education (ACCME) shares resources to support DEI in accredited education, by highlighting opportunities like the National Health Equity Grand Rounds series and the “DEIA Tools for CE Professionals” course in the ACCME Academy. A survey conducted across a host of national nursing organizations (NNOs) analyzed NNOs’ availability of policies and clinical resources on DEI to engage, educate, and equip nurses to deliver patient-centered, culturally responsive care and to effectively recognize and respond to implicit bias in healthcare settings.
The Accreditation Council for Pharmacy Education (ACPE) has developed a guide to emphasize various ways to incorporate DEI at both the organizational and activity levels. Preparing a diverse workforce skilled at caring for diverse populations is essential for achieving health equity in our society. All groups actively encourage the submission of external DEI resources to expand the collective library of materials for the healthcare education community. Accrediting organizations reflect a dedication to fostering a more inclusive and equitable environment for healthcare professionals through education and resource sharing.
What is DEI?
By definition, DEI is a proactive set of values, practices, and/or programs. It is designed to apply a strategic framework in order to promote:
- Diversity in terms of representation (people and perspectives) (ie, being cognizant of who is at the table)
- Equity by ensuring fairness in access and opportunity
- Inclusion by creating a welcoming environment where everyone belongs (via power, voice, and organizational culture).
A Very Brief History Lesson
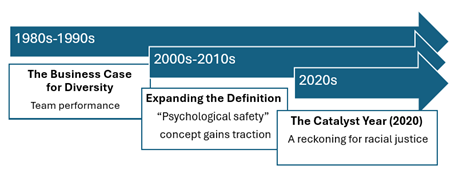
The roots of DEI explicitly emerged in the 1960s, when the United States was deeply segregated. Up until that time, discrimination in hiring, housing, education, and public life was legal in many places. DEI was developed to address a serious problem in the workplace: unequal access to opportunity.
The focus of DEI was on correcting a long-standing imbalance and ensuring fair treatment. It evolved beyond compliance in the decades that followed.
The original goal of DEI was to heighten awareness of the need for equal access to opportunities. It was designed to foster and advance a merit-based system and it was never intended to suggest that employers must hire or advance unqualified candidates, which is a common misperception. In CPD, we must consider who has access to professional development opportunities.
The aim of DEI programs is not merely to design inclusive systems, but to create environments where people say, “I feel like I belong here.” In that spirit, some organizations have opted to add the letter “B” (for belonging) to further strengthen the organizational culture component of their DEI framework. Belonging goes one step further, as it emphasizes the emotional and psychological experience of being accepted, valued, and safe to be oneself within a group or organization. As education professionals, we know about the importance of psychological safety in healthcare settings. Adding “B” for belonging is part of a broader shift from policy and metrics toward lived experience and organizational culture, which is an important element.
Stated bluntly, the work conducted by healthcare professionals is “a big thing,” and the stakes are high. Patients’ lives and their quality of life are directly impacted by the interactions they have with the healthcare system and staff. Ensuring a sense of belonging can have a huge impact.
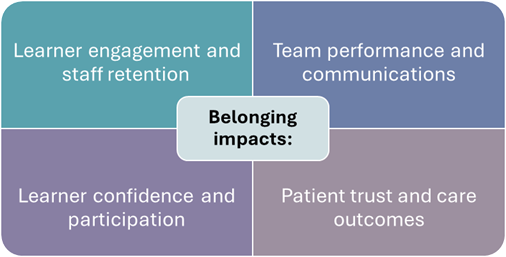
The elements in the DEI framework play an important role in supporting a positive environment. Healthcare professionals must be guided to provide evidence-based, timely, tailored solutions to address the complex needs of patients and caregivers. A properly applied DEI strategy could positively contribute to meeting a healthcare organization’s overall objectives to fully utilize and align their talent pool in the best interest of their patients.
Research in the value of interprofessional education highlights the importance of establishing a positive, productive, and welcoming work environment that leverages the best from all who participate in the decision-making and delivery of services. The complexities found in healthcare (eg, diverse patient populations, social determinants of health leading to access to care barriers, inconsistent screening and untenable treatment plans) all call for innovative strategies that require collaborative practice and engagement.
Why DEI Still Matters
DEI within the healthcare community requires professionals to identify and address care gaps that exist. We must strive to implement strategies for continuous improvement by creating systems whereby we position all members of the care team to succeed. It is critical we consistently deliver professional development opportunities designed to improve upon healthcare professionals’ ability to care for their patients.
Despite the criticism, DEI continues to address urgent and measurable gaps. The care provided to a diverse patient population (and their caregivers) is highly-dependent upon appropriately aligned, skilled healthcare professionals working together toward common goals. As it stands, the healthcare equity gaps that exist are undeniable and remain, unfortunately, far too persistent. The positive impact of effective collaboration and coordination across all members of the interprofessional healthcare team has been demonstrated in numerous healthcare settings and via a growing number of impactful quality improvement initiatives.
Looking Ahead
In the spirit of improved patient care, reflect on your approach to CPD initiatives. What steps are you taking to ensure fair and equal access to relevant professional development opportunities?
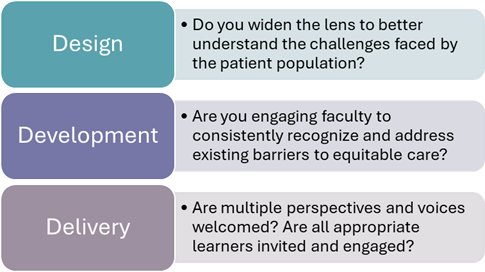
Instead of retreating from DEI, organizations can make thoughtful moves to advance their initiatives. The future of DEI calls for expansion of inclusion efforts to be more transparent, participatory, and accountable. The success of DEI depends on disseminating meaningful communications, moving past slogans, and ensuring substantive and sustainable changes are implemented, monitored, rewarded, and celebrated.
Here are four recommended actions and/or design practices that could help support successful DEI efforts.

The goal is not to silence disagreement, but to create space for learning. When done well, DEI is not about division; rather, it is about collaboration and respect. It is about creating systems where everyone can succeed; the ultimate result is our diverse patient population receives better care. Now, who could argue with that?
Perhaps the acronym should stand for “Dignity for Every Individual”.
“Diversity and inclusion are about giving value to every human being, no matter our differences.”
 Ginny Jacobs, PhD, M.Ed., MLS, CHCP, FSACME, FACEHP, has more than 30 years of organizational development, educational planning, human resources, accreditation experience and system thinking across a wide range of corporate and academic settings. She has extensive experience as a change agent delivering education consulting services focused on improving the performance of healthcare teams and addressing the need for safe, high-quality patient care. She serves on the editorial board for Journal of Continuing Education in the Health Professions (JCEHP) and she is the current chief editor of SACME’s CE News. She holds two master’s degrees (one in education and one in the study of the use of technology in corporate training programs) and a PhD in organizational development. Jacobs is the executive director of Quality Catalyst Group, an independent consulting firm focused on workforce and strategic planning.
Ginny Jacobs, PhD, M.Ed., MLS, CHCP, FSACME, FACEHP, has more than 30 years of organizational development, educational planning, human resources, accreditation experience and system thinking across a wide range of corporate and academic settings. She has extensive experience as a change agent delivering education consulting services focused on improving the performance of healthcare teams and addressing the need for safe, high-quality patient care. She serves on the editorial board for Journal of Continuing Education in the Health Professions (JCEHP) and she is the current chief editor of SACME’s CE News. She holds two master’s degrees (one in education and one in the study of the use of technology in corporate training programs) and a PhD in organizational development. Jacobs is the executive director of Quality Catalyst Group, an independent consulting firm focused on workforce and strategic planning.
 Pam McFadden, FACEHP, FSACME, has over 30 years of experience in continuing professional development (CPD) in healthcare. She has created optimal provider/patient education, inspiring teams by aligning strategic direction with organizational priorities and developing innovative methods to assess outcomes of continuing education (CE) activities. She has been past president of the Society for Academic Continuing Medical Education and the ACEHP. McFadden applies a system-thinking perspective to navigate the complexities of healthcare education, recognizing the voices of both providers and patients. McFadden led the outreach program at UNTHSC, offering strategic academic CE to healthcare professionals throughout Texas and the U.S. Following her “retirement” from UNTHSC, she worked for an educational/performance improvement research-based company and a government workforce solutions organization. McFadden’s commitment to community service includes participation on numerous advisory boards, DFW AHEC, Fort Worth Safe Communities Coalition, and NorTEX, and co-founding the DFW Birthday Brigade, a foundation focused on foster children.
Pam McFadden, FACEHP, FSACME, has over 30 years of experience in continuing professional development (CPD) in healthcare. She has created optimal provider/patient education, inspiring teams by aligning strategic direction with organizational priorities and developing innovative methods to assess outcomes of continuing education (CE) activities. She has been past president of the Society for Academic Continuing Medical Education and the ACEHP. McFadden applies a system-thinking perspective to navigate the complexities of healthcare education, recognizing the voices of both providers and patients. McFadden led the outreach program at UNTHSC, offering strategic academic CE to healthcare professionals throughout Texas and the U.S. Following her “retirement” from UNTHSC, she worked for an educational/performance improvement research-based company and a government workforce solutions organization. McFadden’s commitment to community service includes participation on numerous advisory boards, DFW AHEC, Fort Worth Safe Communities Coalition, and NorTEX, and co-founding the DFW Birthday Brigade, a foundation focused on foster children.