Social media (social media) platforms can play an important role in announcing new and important findings to the scientific community and allowing healthcare professionals (HCPs) to share ideas. Opportunities for peer-to-peer exchange, particularly among members of the interdisciplinary team, can be limited in traditional medical education formats. Social media eliminates barriers, encouraging and fostering thoughtful exchange across the healthcare team. With the limitations often placed on the critical appraisal and delivery of new findings in medicine typically reserved for medical conferences and commentary by a handful of experts, leveraging social media can fill an important gap in the timeliness of distributing information and cultivating the exchange of ideas. The use of social media as a teaching and adult learning tool in medical education offers a dynamic method for including students and trainees in the development of their own knowledge and facilitating engagement, self-reflection and active learning.
Unfortunately, limited evidence and program outcomes from CME/CE activities natively hosted on social media channels have been formally published. This article aims to provide evidence of impact from a multi-pronged, CME-certified, social media-hosted initiative focused on Short Bowel Syndrome (SBS).
Educational Topic
Short bowel is characterized by the physical or functional loss of a significant portion of the small intestine. SBS is a complex clinical condition that occurs from reduction/loss of intestinal absorption. Symptoms of SBS vary according to the extent of bowel loss, but can include diarrhea and fatty stools, fatigue, weight loss, malnutrition, abdominal pain and dehydration. (Jeppesen et al., 2014) The degree of SBS can range from intestinal insufficiency — in which the functional capacity of the gut is reduced but the patient does not require parenteral nutrition (PN) to maintain health — to intestinal failure — where the function of the gut is reduced to a point that is below the minimum necessary for the patient to absorb adequate macronutrients, electrolytes and water, requiring PN (as well as IV) supplementation. (Kim et al., 2017)
However, PN itself is associated with complications. Management of patients with SBS has been bolstered by the recent addition of the agent teduglutide. With multiple treatment modalities available, combined with the unique challenges associated with this condition, it is becoming increasingly understood that patients with SBS are best managed under a model of coordinated care. (Matarese et al., 2014) Clinicians treating patients with this rare condition need to be aware of current recommendations and best practices to ensure optimal care for those patients.
Format
Bonum Continuing Education (Bonum), in partnership with MondayNightIBD, developed an initiative to capitalize on the real-time nature of social media and to fulfill an urgent need in current medical practice by delivering up-to-date education in accessible, engaging and innovative formats. “The Long and Short of It: Optimizing Patient Care in Short Bowel Syndrome” relied on a tiered approach to education utilizing the following learning approaches; knowledge, problem-based and performance.
Three Twitter/X-based Tweetorials and video-based activities served as the knowledge-acquisition portion of the program. Tweetorials are a collection of threaded tweets that utilize text, graphics, polling questions, video, etc., through a linear progression of ideas that teach key concepts.
Three Twitter/X, YouTube, Instagram and traditionally hosted video activities exposed learners to key questions in clinical practice for patients with SBS and discussed nuances of patient management in different clinical settings.
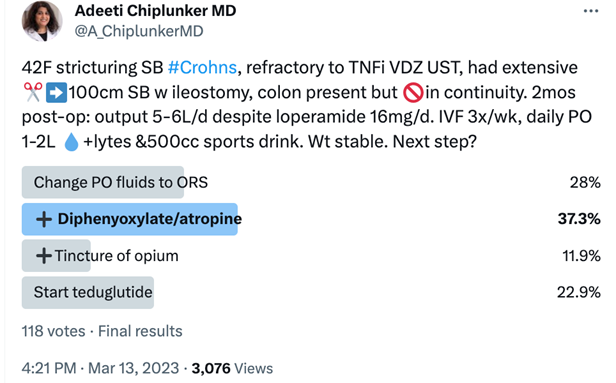
Three MondayNightIBD Clinical Case Conversations allowed learners to apply their knowledge, competence and skills. Clinical Case Conversations are Twitter/X-based group chats that explore the care of a standardized patient. A guest moderator presents a short case vignette with a polling question and four possible clinical actions. These actions are all feasible clinical options, highlighting the grey area of practice, allowing navigation of care preferences for both patients and HCPs.
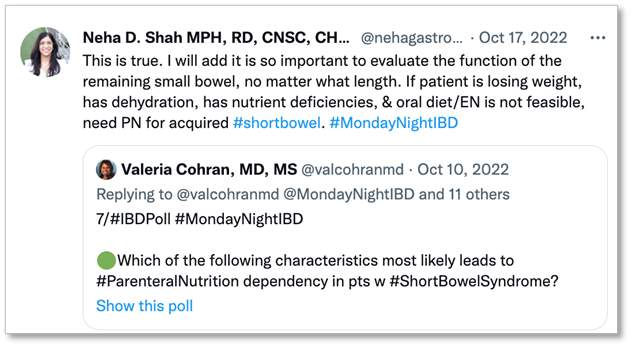
Similar to the Clinical Case Conversation, one MondayNightIBD #PatientExperience Conversation was conducted with two patient leaders serving as guest faculty probing patient preferences. The lead-in tweet from this #PtExperience conversation and one of the Clinical Conversations can be seen below.
A patient case simulation (hosted on both social media and traditional CE hosting sites) is scheduled to launch in January 2024.

The program aims to help clinicians:
- Identify the role and complications associated with the use of PN in patients with SBS.
- Interpret referral and treatment strategies to optimize a patient’s likelihood of achieving intestinal rehabilitation.
- Select pharmacologic options for treatment of patients with SBS.
SBS Care Team and Program Target Audience
Most clinician experience with SBS occurs in specialized centers known as intestinal rehabilitation centers or programs (IRCs or IRPs, respectively). IRCs are major medical centers that have available the interdisciplinary teams with the experience that allows for centralized, integrated management of SBS. [Storch et al., 2014] However, there are only 18 adult IRCs and 21 pediatric IRCs available in the United States, and access to IRCs is often an issue for patients. Thus, gastroenterology HCPs outside of these centers need increased familiarity with the appropriate management of SBS. (Wall et al., 2021)
Inflammatory bowel disease (IBD) increases the predisposition of SBS, particularly for patients with Crohn’s disease, often because of surgical intestinal resection(s). The target audience of this program included IBD specialists, gastroenterologists, surgeons, social workers, dietitians, pharmacists, nurses, nurse practitioners, physician associates/physician assistants, pediatricians, internists, psychologists, and feeding therapists.
By partnering with digital opinion leaders and influencers in SBS, Bonum ensures the content reaches a relevant audience of engaged clinicians, patients and caregivers.
MondayNightIBD is an online IBD discussion forum created by Aline Charabaty, MD. This open-access, virtual CME program engages the global IBD and gastroenterology community on X (formerly known as Twitter). In a revolutionized grand-round style, every other Monday, a guest moderator virtually presents a case vignette to a group of IBD specialists, gastroenterologists and trainees on X. Cases are designed to address the “grey areas” in IBD; focusing on patient cases that fall outside the guidelines and/or provide complex challenges in IBD management. The guest moderator and permanent program moderator (Dr. Charabaty) drive discussion among participants by asking questions, providing feedback, offering resources and helping the group reach consensus in a crowdsourcing educational platform. Additional weekly programming elements include #Back2Basics Tweetorials, which provides a knowledge-based primer the week prior to the Case Conversation; #PatientExperience Conversations, which engage the online community of patients with IBD; and the #IBDAlgorithm, which summarizes the current evidence and group discussions in a handy, one-page format.
Progress
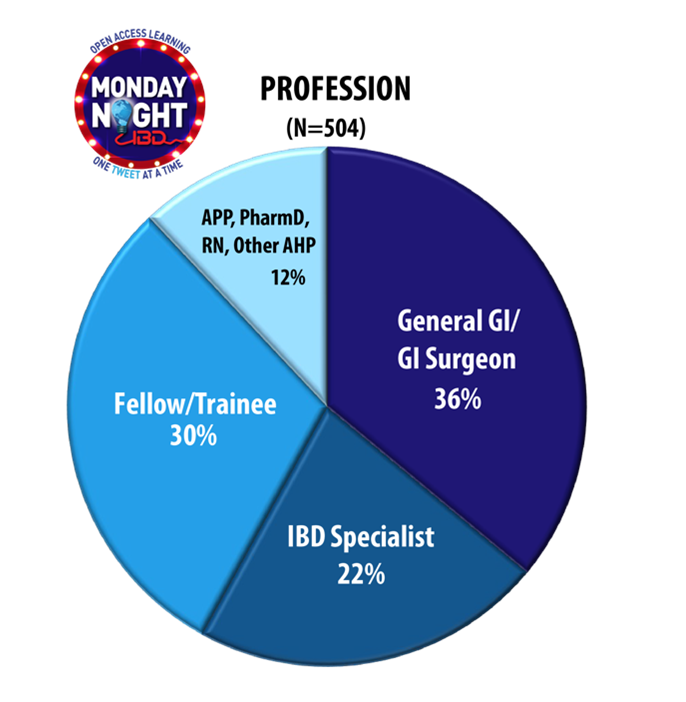
The program, which includes 11 unique activities, included launches spread across 2023. Data from the first five activities indicate high interest and engagement, with over 24,000 unique viewers and more than 1,500 learners advancing beyond the pre-survey. For those whose demographics could be collected, the distribution of professions across the care team is illustrated in the pie chart below:
Outcomes
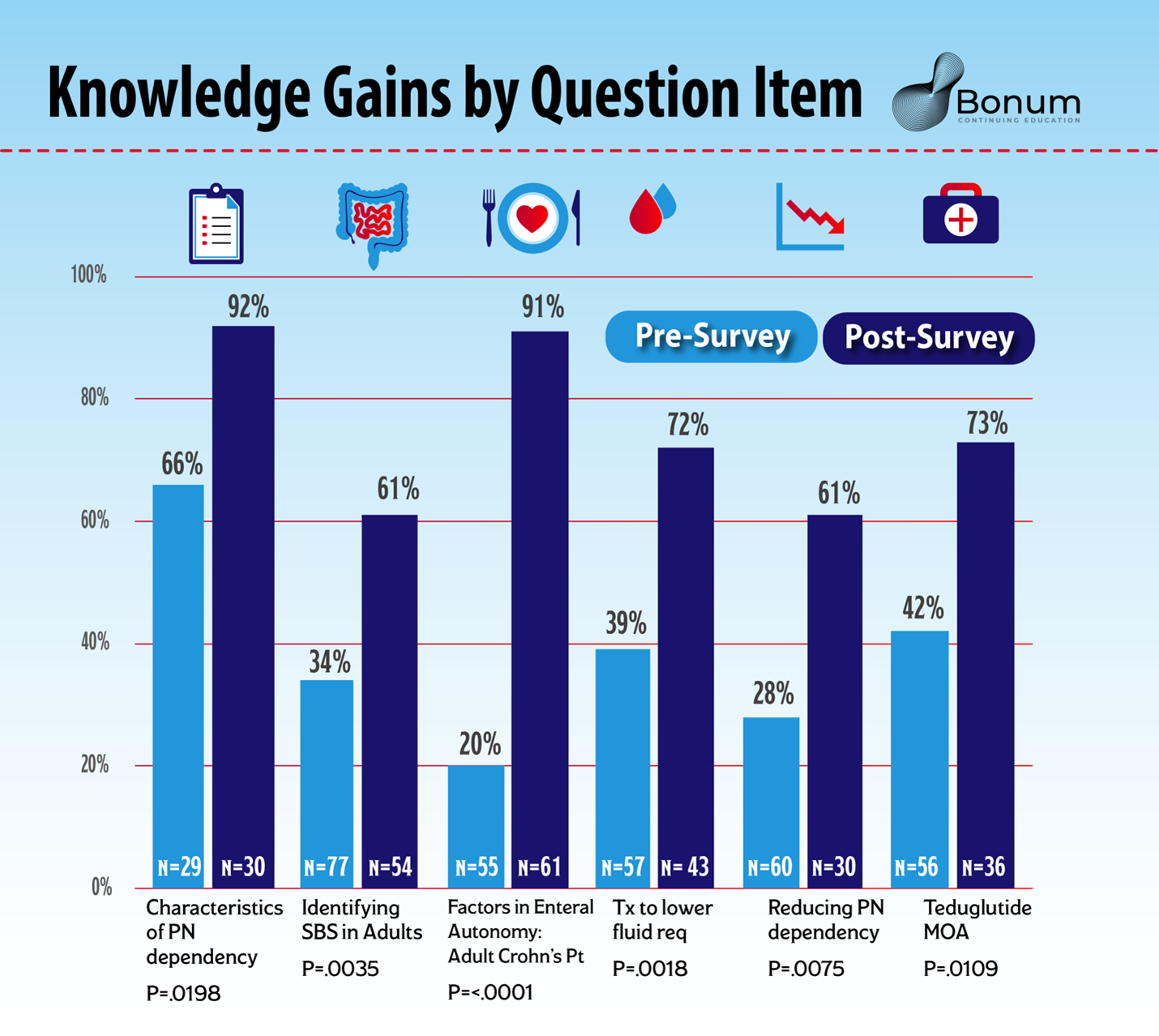
Learners showed significant knowledge improvement on the first five activities across multiple question items. Non-matched pre- and post-samples were analyzed for significance using a chi-square test. Sample sizes (n) ranged from 23 to 77. Across 16 unique question items, more than half of the question items returned chi-square P value < 0.05. To date, the average pre-test score across all question measures is 49%, and the post is 74% (Delta is 25% with a relative improvement of 51%). The largest gains are seen in the learner’s ability to identify characteristics of pediatric and adult SBS, factors contributing to PN dependency and therapeutic options for various patient cases.
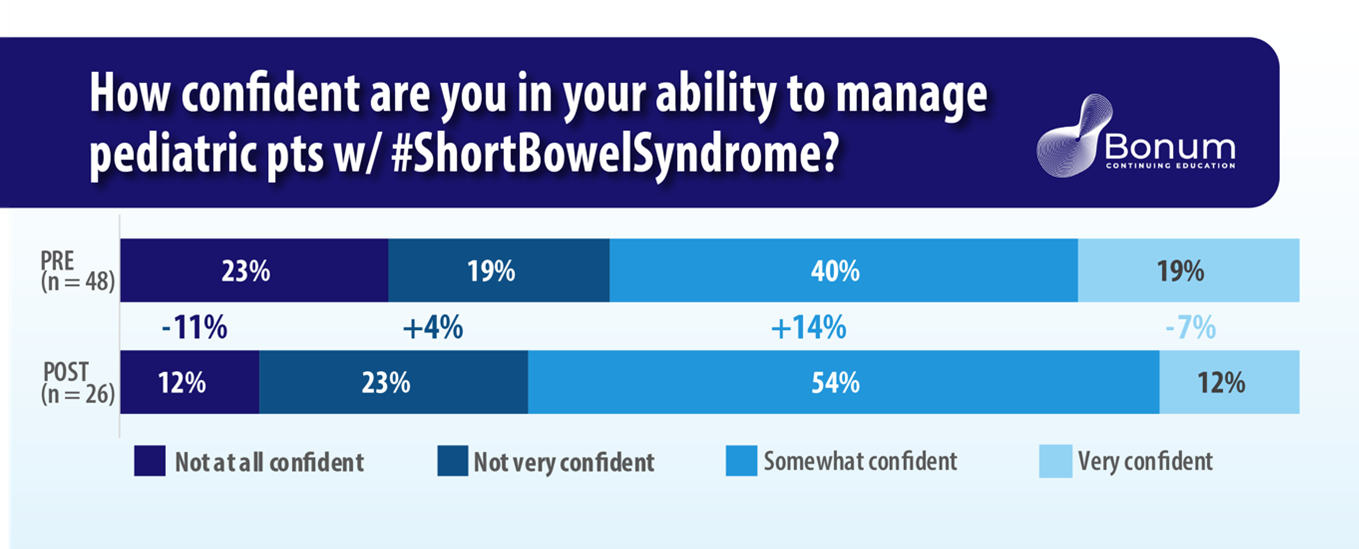
A pre-/post-confidence measure indicated further education is needed on this topic. Respondents showed a lower percentage, selecting “very confident” in managing pediatric patients with SBS from pre-test to post-test (19% to 12%). “social media what confident” showed a 14% increase, indicating learners moved away from lower confidence categories and a high degree of confidence, converging in an overall moderate level of confidence. This may suggest that a portion of the learner group was not cognizant of their own gaps and, therefore, believed themselves to be more informed prior to taking the education, then recalibrated their sense of confidence on the post-test question.
The interim outcomes for this program show significant improvement in knowledge, which — if extrapolated over the 504 total trackable learners who participated in one or more of the activities — may have a far-reaching impact on both clinicians and their patients. Continued data collection and analysis on future activities are expected to show similarly significant gains in competence and confidence.
Impact
Due to the nature of social media platforms’ functionality, capturing polling responses can be more challenging than in traditional medical education formats. Additionally, the relatively rare nature of SBS impacts the number of providers seeking education on this topic. However, initial results have shown statistically significant (p<.05) knowledge gains, even with small samples (n values ranging from 23 to 77). Specifically, knowledge and competence gains were measured with regard to identifying the role and complications associated with the use of TPN in patients with SBS, as well as interpreting referral and treatment strategies. Further competence data will be collected in the simulation activities. Data will be aggregated and analyzed by topic, Moore’s level and activity type.
Further, owing to social media ’s broad reach and the program’s robust curriculum, continued outcomes demonstrating statistically significant improvements across learning domains are expected. This program’s design creates multiple opportunities to collect data from learners over a period of several months, allowing for analysis of clinician gains over time.
There is ongoing discussion in the continuing medical education community regarding the relative value of social media as a vehicle for distributing certified education. This program highlights the opportunity created by social media to conduct relevant medical education and overcome barriers experienced in the traditional setting. In an effort to reach treaters of a rare condition, social media was used to leverage the wide professional following by established thought leaders. The format encourages a more democratic discussion among the care team and has shown that it can deliver statistically significant learning gains on par with traditional educational formats. As medical education providers strive to lower barriers to information and meaningfully engage learners, the potential of social media cannot and should not be dismissed.
 Angelique Vinther, CHCP, has been an active professional and leader in the CME/CE industry for 15 years, specializing in outcomes analysis and reporting. She primarily focuses on collection/analysis methodologies, data transparency, test question-writing best practice and clear messaging. Her consulting business supports educational providers with a range of services, allowing her to use outcomes data to tell different types of stories for different audiences. She is active in the CPD community as a mentor, volunteer and, most recently, treasurer for the Colorado Alliance for Continuing Medical Education (CACME).
Angelique Vinther, CHCP, has been an active professional and leader in the CME/CE industry for 15 years, specializing in outcomes analysis and reporting. She primarily focuses on collection/analysis methodologies, data transparency, test question-writing best practice and clear messaging. Her consulting business supports educational providers with a range of services, allowing her to use outcomes data to tell different types of stories for different audiences. She is active in the CPD community as a mentor, volunteer and, most recently, treasurer for the Colorado Alliance for Continuing Medical Education (CACME).
 Allison Kickel, FACEHP, is the founder and president of Bonum Continuing Education, an independent medical education company. She has spent the past 15 years in the world of CPD focusing primarily on educational strategy, business development and program innovation.
Allison Kickel, FACEHP, is the founder and president of Bonum Continuing Education, an independent medical education company. She has spent the past 15 years in the world of CPD focusing primarily on educational strategy, business development and program innovation.
An active member of the CPD volunteer community, Allison currently serves on the Alliance Annual Conference and Membership Committees. She is also the casual gatherer of Colorado-based CPD folks for regular happy hour events.
In addition to her professional and volunteer roles in the industry, Allison is an avid traveler, reader and all-around curious soul.
Funding for this program was provided through an independent educational grant from Takeda Pharmaceuticals, Inc.
References
Breu AC, Abrams HR, Manning KD, et al. Tweetorials for Medical Educators. J Grad Med Educ. 2021 Oct;13(5):723-725
Breu AC. From tweetstorm to tweetorials: threaded tweets as a tool for medical education and knowledge dissemination. Semin Nephrol. 2020;40(3):273–278. doi: 10.1016/j.semnephrol.2020.04.005.
Jeppesen PB. Spectrum of short bowel syndrome in adults: intestinal insufficiency to intestinal failure. JPEN J Parenter Enteral Nutr. 2014;38(1 Suppl):8S-13S.
Jeppesen PB. Pharmacologic options for intestinal rehabilitation in patients with short bowel syndrome. JPEN J Parenter Enteral Nutr. 2014;38(1 Suppl):45S-52S.
Kim ES, Keam SJ. Teduglutide: a review in short bowel syndrome. Drugs. 2017;77(3):345-352.
Matarese LE, Jeppesen PB, O'Keefe SJ. Short bowel syndrome in adults: the need for an interdisciplinary approach and coordinated care. JPEN J Parenter Enteral Nutr. 2014;38(1 Suppl):60S-64S.
Storch KJ. Overview of short bowel syndrome: clinical features, pathophysiology, impact, and management. JPEN J Parenter Enteral Nutr. 2014;38(1 Suppl):5S-7S.
Wall E, Lakananurak N, Pevny S, et al. Gaps and opportunities in the management of short bowel syndrome: an international inquiry. JPEN J Parenter Enteral Nutr. 2021;45:S44–S240. Abstract P122.