Introduction
The translation of clinical research to practice has been the subject of intense scrutiny in efforts to identify ways to improve uptake of findings that can enhance patient care. In this study, we evaluated the experience of nephrology healthcare providers who manage patients with autosomal dominant polycystic kidney disease (ADPKD) as they strive to translate research results into clinical practice.
ADPKD is the most commonly inherited renal disorder and affects up to 600,000 people living in the United States and 12 million people worldwide. This painful and life-threatening disease is the fourth leading cause of end stage renal disease. Patients with ADPKD experience a relentless growth of cysts leading to enlargement of the kidney and, ultimately, to kidney failure.
The study identified factors that may enhance or impede research translation in nephrology settings. The study authors were Dana Ravyn, PhD, MPH; Beth Goodwin, MA; Rob Lowney, MBA from CMEology and Arlene Chapman, MD, professor of medicine from The University of Chicago. The study was supported in part by a grant from Otsuka America Pharmaceutical, Inc. The funders of this study had no role in the study design, collection, analysis and interpretation of data, writing the report or the decision to submit the report for publication. Results of the study were published in Kidney Medicine. The article is available here.
Activity Overview and Study Participants
Nephrology clinician volunteers (12 MDs and one NP) who took the online continuing education activity, “Strategies to Improve Management of ADPKD: Navigating Pitfalls and Overcoming Challenges,” participated in semistructured interviews. The activity framework consisted of two online modules. At the beginning of the activity, learners were asked four questions to assess their knowledge and competency specific to the management of patients with ADPKD. Learners were seamlessly directed to the module that was most aligned with their needs. The activity was available for 12 months on Healio.com and freeCME.com and was jointly provided by Medical Education Resources and CMEology. On completion of the activity evaluation, participants were asked if they wanted to volunteer to participate in an interview on the translation of clinical results to patient care. An independent institutional review board found the study to be exempt as an educational survey.
Methods
A qualitative study was implemented using inductive thematic analysis to assess the experience of physicians in the evaluation and translation of research findings into clinical practice for the care of patients with ADPKD. Interview questions embraced several methods, including hypothetical (Do you think that…?), provocative (It’s believed that … what do you think?), ideal (What would be a solution to…?) and interpretive (What do you mean by…?). The interview was dynamic and focused on the interviewee’s experiences, opinions, feelings and knowledge while also soliciting input. While survey questions were partially refined based on the interview results, the conceptual framework of the interviews was preserved throughout data collection.
Deidentified transcripts were coded and excerpted, and emergent themes and relationships were identified through analysis performed using Dedoose software. Particular attention was paid to characterizing facilitators and barriers to research translation at different levels of the healthcare environment.
Results
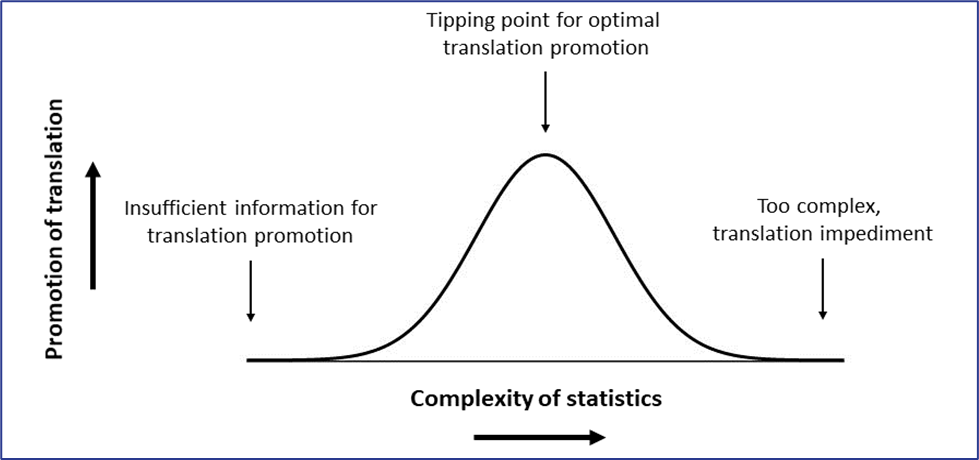
Inductive thematic analysis of the interview data revealed factors that facilitate uptake of ADPKD research in clinical care as well as others that impede those processes. Although well-established barriers to research translation are prevalent among healthcare providers managing patients with ADPKD, these clinicians face unique challenges. Our study found that some factors can both enhance or impede research translation. The influence of these identified factors exists on a continuum, and there is a threshold or “tipping point” above and below which promotion will be more or less effective, respectively.
In the example below, the learner seeks statistical data to interpret implications for care. Understanding the implications for care is difficult if statistical data are inadequate (left). Optimally, some statistical findings such as P values, number needed to treat and number needed to harm can promote understanding and make translation more likely (center). When statistics pass the tipping point where they become overly complex and difficult to interpret clinically, the factor becomes an impediment to translation (right).
Challenges
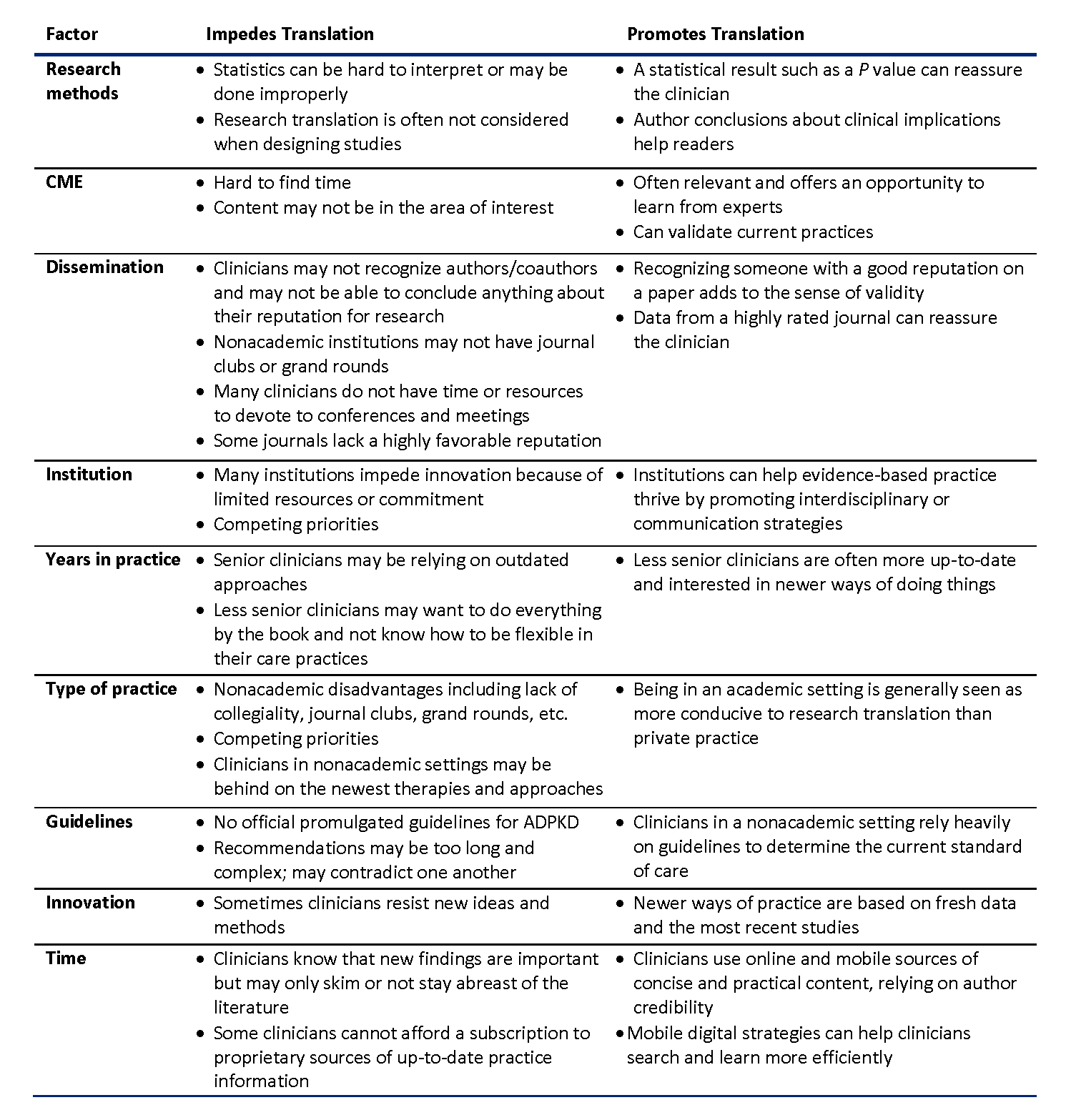
We found several recurring themes that are common to translational science in many areas of clinical practice. These include the quality and quantity of research, institutional and noninstitutional structural factors, dissemination or findings, practice type and sociocultural characteristics of the work environment. Challenges included poor comprehension of complex research reports, difficulty with statistics and the lack of an organizational culture that promotes uptake of new research results. The central challenge specific to ADPKD research translation is the lack of official guidelines. For ADPKD, continuing educational activities played a key role in facilitating research translation by providing evidence-based standards of care in a way accessible by community nephrologists. These factors differed based on the practice setting, in this case academia versus community practice. Below are quotes from study participants.
Academia Compared to Community Practice
“…That’s not what the private practice is about at all … you go in, you see a lot of patients, you try to follow the standards of care … I’m trying to stay up to date with the most recent treatment options … but there is a big difference between [me and] an academic person practicing ... you don’t just go and read literature.” —Physician study participant
“You know, when you're in that academic environment, people constantly push you to look at the data, and I'm not sure that happens as much in private practice. So if there could be simpler algorithms for people to follow, I think that would be helpful.” —Physician study participant
“When you’re in private practice, you don’t have time or expertise to understand all the details of an original manuscript … and that makes it really granular for them to know how to deal with this.” —Physician study participant
Factors That Can Promote or Impede Research Translation into Clinical Practice in ADPKD are outlined below:
Additional quotes from study participants include:
Statistics
“I think that the hardest part to understand of a study is probably the statistics and all the math involved; that sometimes loses one, especially. So I would say that's what distracts the most….” —Physician study participant
“People have concerns that the statistics may not have been done properly in the first place, but they don’t know how to figure that out…” —Physician study participant
Training and Education
“Some of our colleagues probably haven’t been trained in a setting where they’ve literally been taught to think critically to evaluate papers.” —Physician study participant
“…People are not interpreting these [studies] because maybe they understand the data, but they just don't know really how to apply it and put it together; what does it really mean for patient care?” —Physician study participant
“I think there should be a bit more education on research. Polycystic [kidney disease] is not so well talked about. We talk about diabetes and hypertension and cancer and stroke, but not much about polycystic kidney disease.” —Nurse practitioner study participant
Continuing Education
“CME programs help ... They’re opening your mind up to other treatments, other possibilities, increasing your knowledge rather than this little narrow path that you follow.” —Physician study participant
“In general, [providers] found [CE] activities they had completed to be highly relevant and a valuable opportunity to learn from experts for both adopting new practices and validating current practice.” —Physician study participant
“I think the information [from this activity] was really objective, and I think it helps to clarify the current studies that are out there. So it kind of summarizes everything.” —Physician study participant
Study Limitations
This study did not explore translation of all levels of research, such as basic science and animal studies, and it was limited to translation of knowledge from clinical studies. The number of participants was limited but found sufficient for saturation.
Implications for the Continuing Education Community
The findings of this study indicate that continuing education is critical in the translation of ADPKD research to improve the diffusion of innovative practices. Continuing education for rare or orphan diseases such as ADPKD should recognize that the same factors can either promote or impede research translation, and identify the tipping point in the transition from facilitator to impediment for individual factors. Importantly, the research from this study indicates healthcare providers depend heavily on continuing education to determine best practices in the management of patients with ADPKD.
 Rob Lowney, principal/managing director of CMEology received a BA from Connecticut College and an MBA from The University of Hartford. He began his career at Eli Lilly & Company in sales in primary care and, later, in neuroscience. Lowney’s other role while working for Eli Lilly was in managed care. In this capacity, he developed disease state and medical education initiatives designed to enhance clinician performance and improve patient outcomes. Lowney has over 25 years of experience in continuing medical education. He has published in numerous journals including The International Journal of Medical Education, JCEHP, Kidney Medicine and Schizophrenia Research. Lowney founded CMEology in 2011 and maintains responsibility for educational strategy and design and operations.
Rob Lowney, principal/managing director of CMEology received a BA from Connecticut College and an MBA from The University of Hartford. He began his career at Eli Lilly & Company in sales in primary care and, later, in neuroscience. Lowney’s other role while working for Eli Lilly was in managed care. In this capacity, he developed disease state and medical education initiatives designed to enhance clinician performance and improve patient outcomes. Lowney has over 25 years of experience in continuing medical education. He has published in numerous journals including The International Journal of Medical Education, JCEHP, Kidney Medicine and Schizophrenia Research. Lowney founded CMEology in 2011 and maintains responsibility for educational strategy and design and operations.