Read more for a closer look at the 2022 Alliance Innovative Format Award Winners.
Translating evidence-based knowledge into practice is recognized as a primary challenge of CME/CE given the diversity of learners and complexity of healthcare delivery systems. While practice guidelines and standards of care offer frameworks for clinicians, ongoing assessments of real-world practice indicate clinicians often fail to follow these guidelines. Moreover, the number and complexity of guidelines, as well as delays in publication, often equate to sub-optimal prioritization of treatment pathways considerate of the latest evidence. This is especially true in cancer care, where the rate of research and treatment approvals often outpace guideline updates and leave even the best of clinicians with unanswered questions.
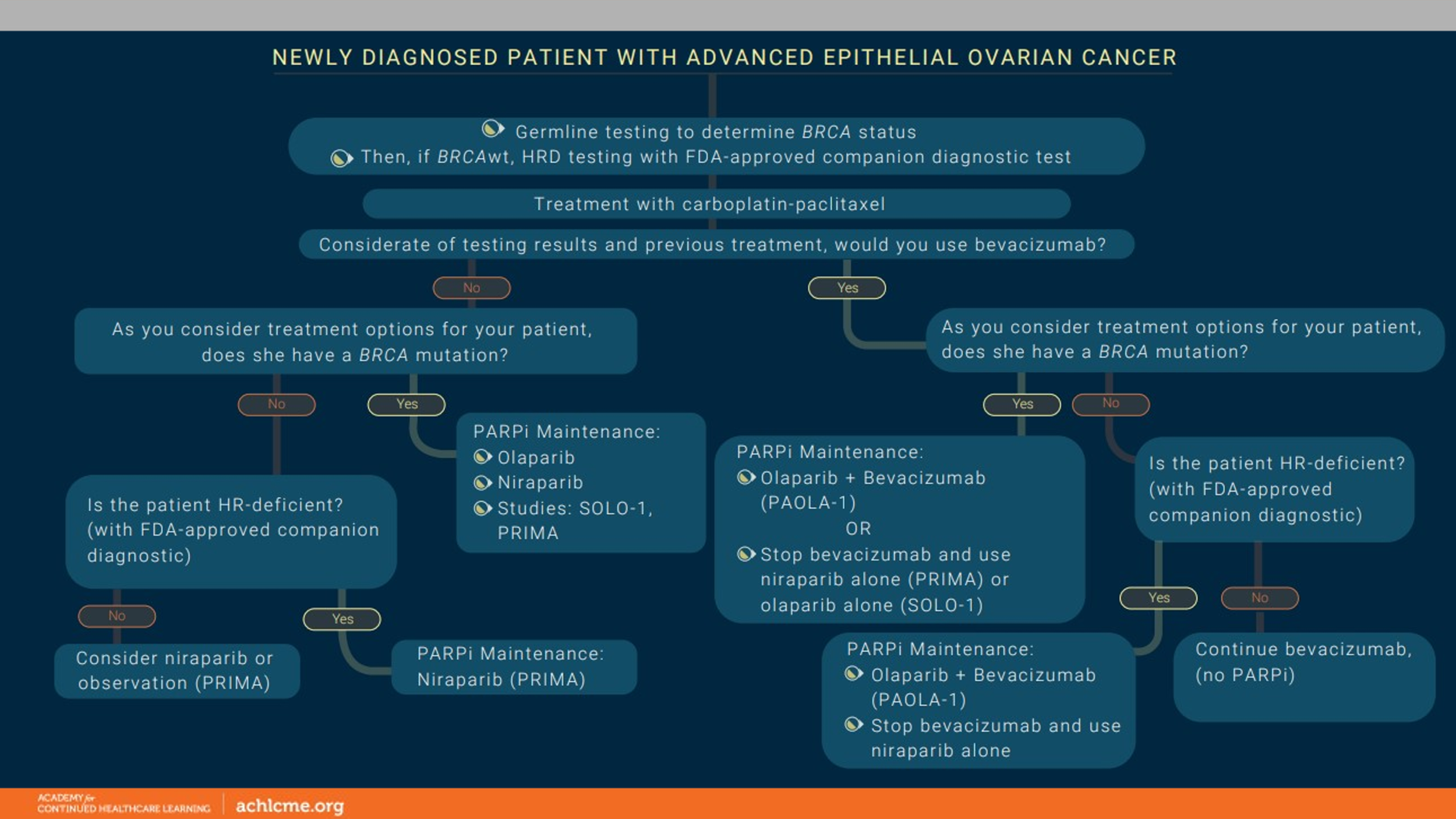
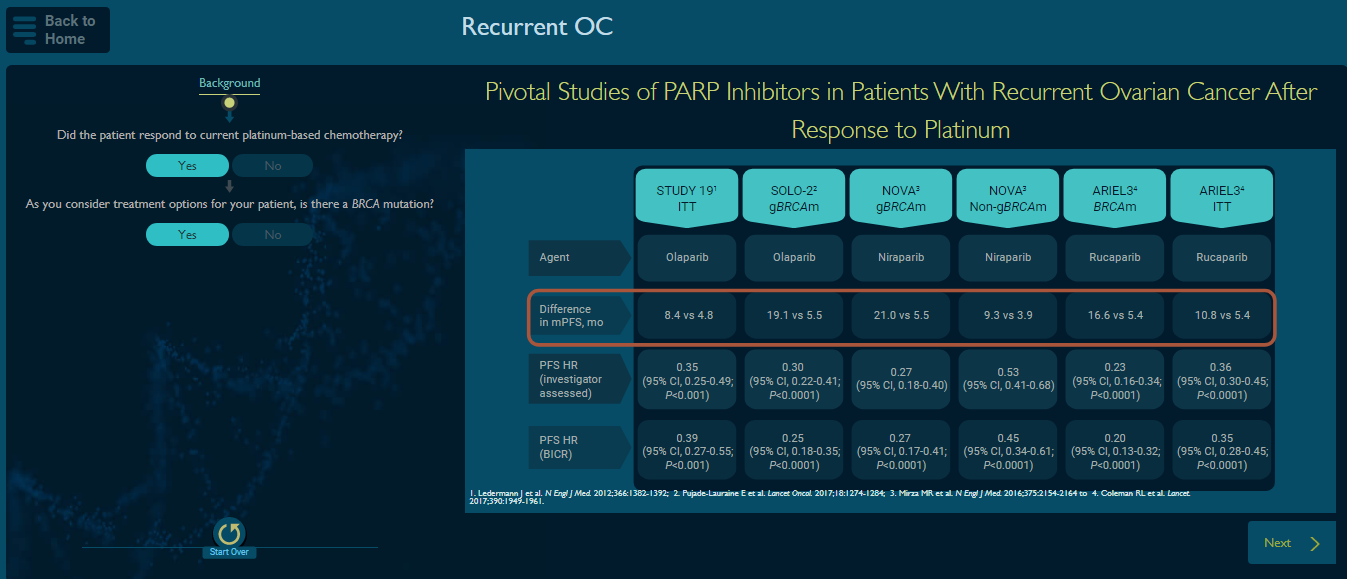
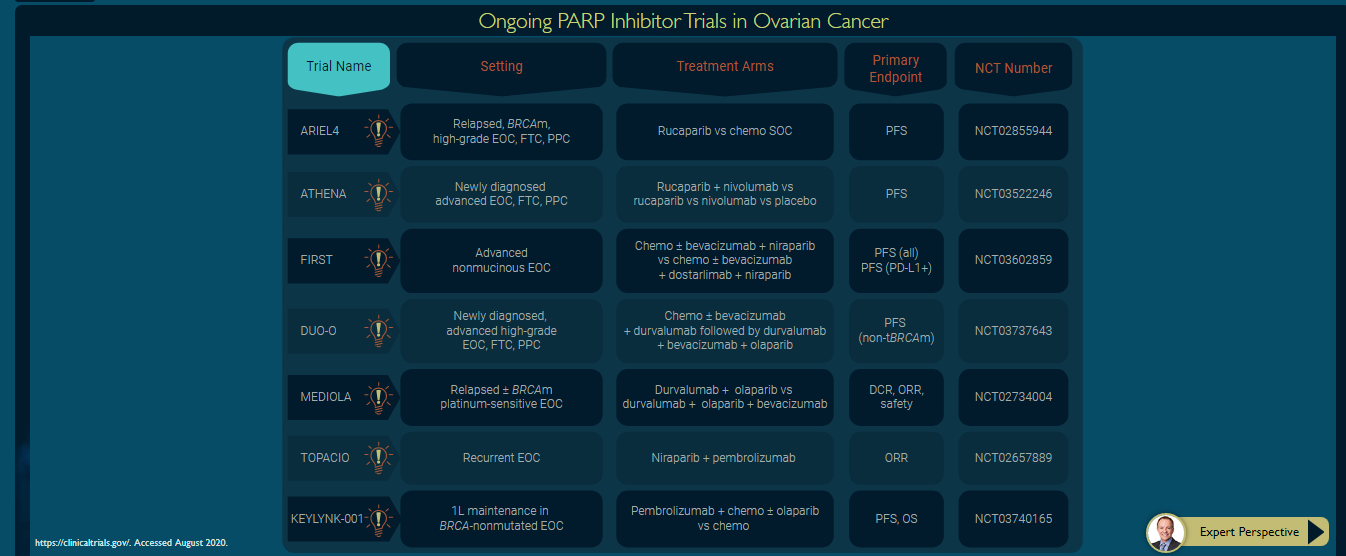
When investigating unmet needs in the treatment of advanced ovarian cancer, we found that PARP inhibitors, a new class of targeted therapy, were not being used optimally to improve patient outcomes. The contributing factors included lack of knowledge and competency on patient selection practices, especially in patients with heavily pre-treated ovarian cancer, and limited clinical experience in managing adverse events associated with these therapies. To address these practice gaps, the educational design needed to simultaneously address deficiencies in disease knowledge, suboptimal treatment selection, inconsistent guideline adherence and inadequate shared decision making (performing precision medicine) considerate of complex and diverse patients.
In light of this, Rush University and the Academy for Continued Healthcare Learning (ACHL) designed a “Pathfinder,” which applies the principles of Mezirow’s transformative learning theory to synthesize and mobilize clinical knowledge in a highly visual way by engaging learners in heightened clinical reasoning and replicating decision making in real-world environments. The learner progresses through the interactive algorithm selecting the biomarkers, patient status and other factors that impact care. These decisions then drive the resultant steps and content. The content within the algorithm uses an infographic design to convey data and expert recommendations. This innovative approach, which blends graphical elements into what is frequently text-based content, yields more effective learning and comprehension. Learners are required to respond to interactive prompts within the algorithm to progress forward. At various points throughout the algorithm, supportive evidence and guidance from expert faculty are provided via video and/or audio clips to reinforce key points and offer additional educational context of the data presented. Lastly, to provide clinicians with a resource to use outside of the digital activity, a downloadable decision tree was included, which could be printed or saved for future reference. The instructional design integrated into this platform applies recommendations from adult learning literature to create an effective and influential learning activity.
This educational design demonstrated significant educational impact, including:
- 80% of the 1,552 learners (OSP-defined) were target audience members (oncologists and oncology nurses)
- An effect size of .81 indicates target audience learners were 48% more knowledgeable/competent post activity (using first-attempt post-test data)
- 115% increase in clinical competency for initial treatment selection in a newly diagnosed patient who is BRCA wild-type
- 138% positive shift in clinical ability to select correct dosage for newly diagnosed patients
- 100% of oncologists post-activity were able to select the most appropriate PARPi for women with recurrent ovarian cancer who have received more than three rounds of chemotherapy
- Oncologists were 22% more confident utilizing PARPis for maintenance therapy and 36% more confident utilizing PARPis for patients with recurrent ovarian cancer
- 71% of learners committed to changing their practice
A full outcomes report can be found here.
Ultimately, the success of this Pathfinder, with avenues for both newly diagnosed and refractory/recurrent patients, stems from its effectiveness in supporting the following learning steps (per the transformative learning theory): self-examination of current approaches to care, critical assessment of how these practices align with recommended pathways, ability to plan a course of action, reinforcement of knowledge and recommendations for best practices to achieve a plan of action, and the ability to apply learnings at the point of care.
To see the functionality of the Pathfinder firsthand, visit the ACHL website.
Rush University and ACHL would like to thank GSK for providing an educational grant to support this important education.