Institutional Affiliation: Zucker School of Medicine at Hofstra-Northwell
Project Description
Northwell Health implemented an initiative to utilize interdisciplinary pre-visit huddle and pre-visit counseling of patients to improve pneumococcal vaccination rates among patients at increased risk of pneumococcal disease between the ages of 19–64 years.
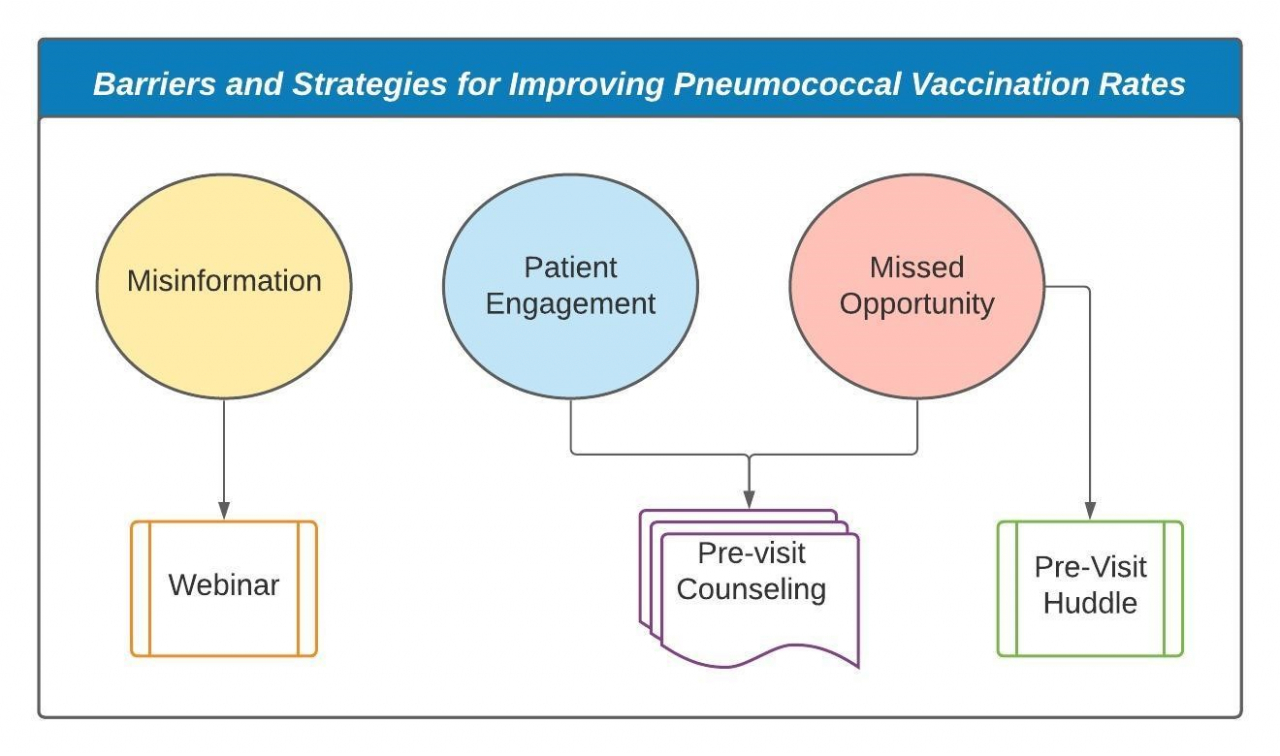
The initiative aimed to address three of the major barriers to immunization as shown in Figure 1 below: misinformation, missed opportunity and patient engagement.1 Misinformation was targeted by using an educational webinar aimed at improving baseline understanding of evidence for clinicians, nursing staff and other members of the interdisciplinary team. In addition, the webinar addressed the efficacy of interdisciplinary huddles and motivational interviewing. The webinar was created in collaboration with the New York Chapter of American College of Physicians (ACP). The faculty of the webinar included physicians, nurse practitioners and nursing leadership, while the audience included nurses, physicians, physician assistants, nurse practitioners, fellows and students. To address missed opportunities for immunization, we implemented the use of a pre-visit huddle between nurses and clinicians within the practice. Patient engagement was addressed by using a motivation interviewing technique to ascertain a patient’s comfort with vaccination during the pre-visit counseling with nurses. Furthermore, clinicians attempted to re-engage using motivational interviewing for those patients who deferred vaccination pre-visit calls.
Figure 1
Process
Nurses were provided a list of patients with upcoming appointments. Nurses then identified which patients qualified to receive the pneumococcal vaccination and initiated pre-visit calls. In the phone calls, nurses identified patients who: 1) previously received the vaccine, 2) deferred the vaccine or 3) were amenable to receiving the vaccine during their visit.
Subsequently, pre-visit huddle was the opportunity for nurses and clinicians to discuss the preference of each eligible patient, with special attention paid to those who were deferring vaccination.
Accomplishments
Through the education webinar, members of the interdisciplinary team received the most recent CDC recommendations for the pneumococcal vaccine. The pre- and post-assessment surveys showed an increase in knowledge for the participants of this webinar. Additionally, compared to before the webinar, participants felt more comfortable with pneumococcal vaccine recommendations for patients, especially for those under the age of 65.
Through the combination of pre-visit counseling and pre-visit phone calls, this initiative increased engagement with patients. In addition, it provided at least two opportunities for patients to ask questions and discuss their concerns. This rapid-cycle quality improvement initiative resulted in a significant increase in vaccination rate in this cohort.
This initiative combined elements of provider education, pre-visit counseling and pre-visit interdisciplinary huddles as a framework for a unique approach to pre-visit planning in non-primary care specialties within internal medicine.
We have submitted our project and findings as an abstract to the American College of Physicians and Society of General Internal Medicine annual conferences. We are currently in the process of writing a manuscript based on our lessons learned. We also plan on disseminating the educational webinar to other institutions.
Challenges
The COVID-19 pandemic caused a delay in the start of this grant-funded project; therefore, the initiative took place over a limited timeframe. In addition, for purposes of social distancing, the nurses were unable to be co-located within the practice for the huddles. Lastly, we suspect that fewer patients were eligible due to loss of insurance and possibly other social determinants of health noted in volume of canceled appointments and patients who were unreachable. Nevertheless, this initiative provided an opportunity to target a cohort at risk of complex morbidities.
Lessons Learned
This quality improvement initiative incorporated a clinician education webinar, pre-visit counseling with nurses and interdisciplinary pre-visit huddles for patients at an increased risk of pneumococcal diseases. Our experience has shown that a framework for a multidisciplinary approach to pre-visit planning in non-primary care specialties within internal medicine can be utilized for other preventative efforts in the future.
References
- Johnson DR, Nichol KL, Lipczynski K. Barriers to adult immunization. The American Journal of Medicine. 2008 Jul;121(7 Suppl 2):S28-35. DOI: 10.1016/j.amjmed.2008.05.005.