Project Description
Patients with rheumatic diseases are at increased risk of invasive pneumococcal disease. Both pneumococcal conjugate vaccine (PCV13) and pneumococcal polysaccharide vaccine (PPSV23) are recommended for patients on immunosuppressant medications. However, under-vaccination is common. The aim of this quality improvement project was to decrease the proportion of veterans due for either vaccination from the baseline of 36% to a goal of 28%. The project is taking place at Tennessee Valley Healthcare System (TVHS) Rheumatology clinic with a goal intervention timeframe of six months.
The intervention had two main components: general education and a targeted clinical intervention. The clinical intervention was deployed in October 2019 with a single provider panel, then scaled to include multiple providers in subsequent months.
The general educational intervention was developed and distributed using QuizTime. QuizTime is an application tool developed through the academic affiliate. Educators create quizzes and send questions to learners via text or email. Learners receive instant feedback and learning resources once they answer each question. A quiz on eligibility and risk status for pneumococcal disease and vaccination was advertised through email communication to all providers in rheumatology and reiterated at a meeting specific to TVHS rheumatology providers.
The clinical intervention incorporated:
1) Patient letters which included an appointment reminder and educational information about risk for pneumococcal pneumonia and vaccination
2) Provider outreach via the electronic medical record
3) Health system components that included a pre-visit list of those due for vaccination provided to nursing staff
A random sample of 15% TVHS rheumatology completed patient visits was obtained each month and chart review conducted. The primary outcome measure was the percent of sampled patients due for a pneumococcal vaccination. Process measures included the number of vaccinations administered. Balancing measures included qualitative feedback from staff.
Results
Baseline (January–October 2019)
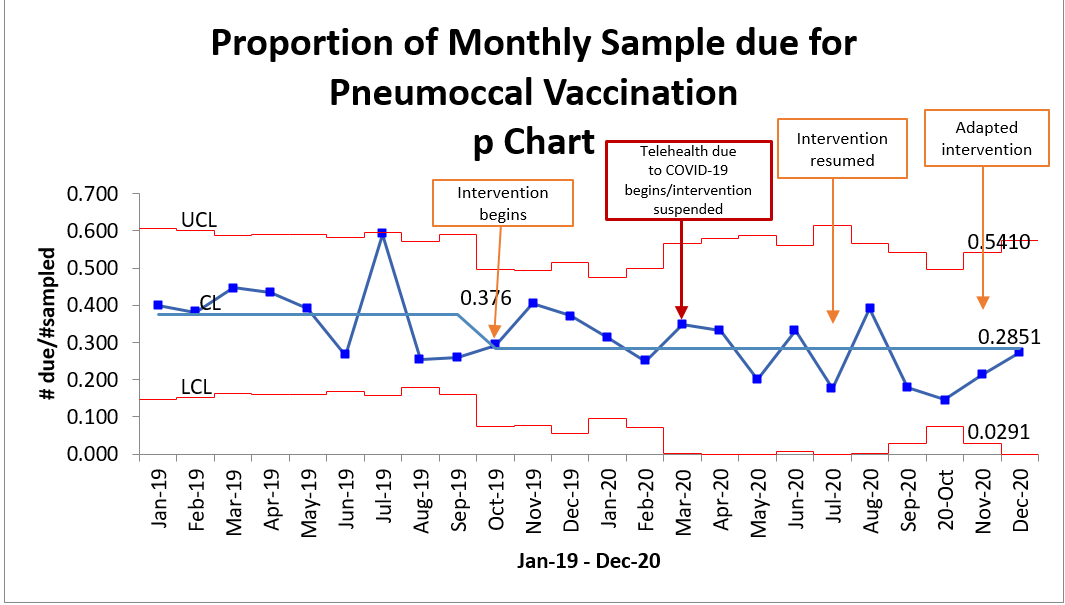
A mean of 37.6% of patients were noted to be due for a vaccine on the basis of age or immunosuppressant use. There was no special cause variation, indicating a stable baseline.
Post-Clinical Intervention (October 2019–December 2020)
One-hundred twenty-one pneumococcal vaccinations were administered in a clinic during this period. An additional 37 vaccinations were administered the same month as data collection, but on dates other than that of the rheumatology visit, indicating perhaps that outreach led patients to seek vaccination during another opportunity in our system. The mean percent of sampled patients due for vaccination has declined to 28.5% overall. There was no special cause variation identified in any of the following sub-periods:
- Intervention start (October 2019–March 2020): Intervention suspended November–December 2019 due to personnel changes. It resumed January 2020.
- COVID Safer at Home (March–June 2020): Clinical delivery shifted to predominantly telehealth. Wider confidence intervals reflect a smaller sample size due to fewer in person visits.
- Intervention resumes (July–December 2020): Intervention resumed with adapted letters mailed which specified
- 1) That a vaccine should be deferred to a scheduled in-person appointment
- 2) The vaccine to be given was not a COVID-19 vaccine. The four consecutive points below the mean (September–December 2020) could be an early change signal, but it is unknown whether this will be sustained.
Challenges
The team faced many challenges throughout the course of the project. First, soon after project initiation, a critical team member died unexpectedly. In the midst of personal grief, each clinician increased their number of patients seen within clinic, further delaying the intervention spread. Second, the COVID-19 pandemic impacted this project in several ways. In March 2020, clinical care was rapidly transitioned to predominantly telehealth delivery following safer-at-home orders. Third, a nursing team member, who is Army reserve, was deployed out of state to assist with the pandemic response. Recently, staff feedback revealed that some patients who had received adapted letters were still presenting unexpectedly to clinic. The intervention was temporarily altered such that letters are not currently being sent to patients. For patients who do have in-person visits, a lead clinic nurse is providing a card denoting vaccinations due, which patients use to engage in discussion with their provider.
Lessons Learned
- Virtual apps such as QuizTime can be used to deliver educational content in a convenient and socially distanced manner.
- Patient and provider outreach through quality improvement can lead to increased vaccination rates in rheumatology clinic.