Acknowledgements: Scarlett, Rice, Katherine Leath, Maria Ruvalcaba, and Rafid Filat for their work on the project.
Project Description
The overall goal was to improve pneumococcal vaccine protection for highest risk patients in the University of Arkansas for Medical Sciences (UAMS) multiple myeloma (MM) and rheumatology clinics. A review of immunization records for patients with multiple myeloma, systemic lupus or rheumatoid arthritis demonstrated that they were not vaccinated against pneumococcal infection at rates recommended in guidelines from the Centers for Disease Control (CDC) Advisory Committee for Immunization Practices (ACIP).
The team planned clinical staff education, patient education and system changes to overcome barriers and improve immunization rates in these target patient populations. The prespecified outcome was to improve pneumococcal vaccination rates in the two clinics by 25% in six months in immunocompromised patients ages 19–64.
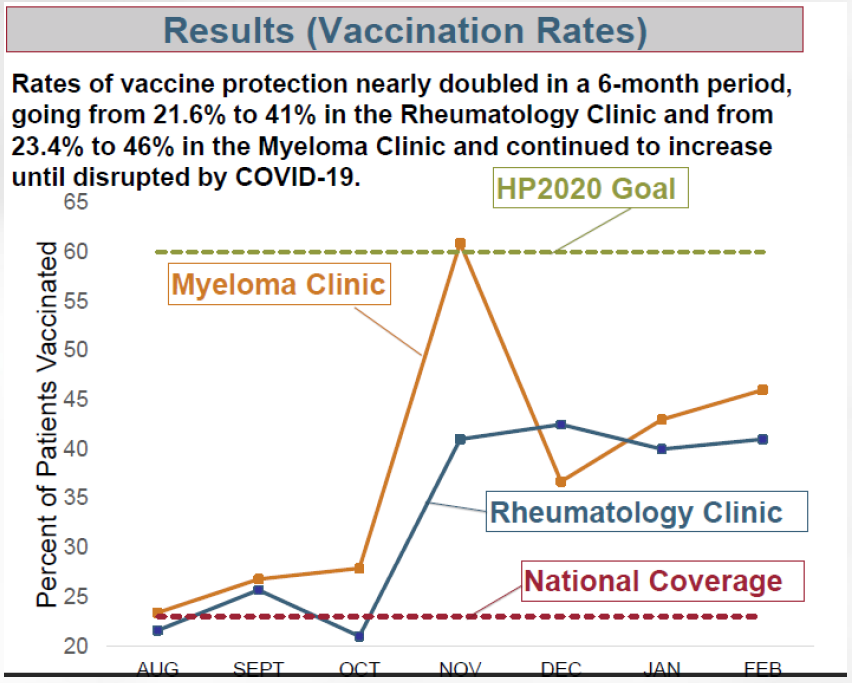
The national coverage rate is 23%1, which is far below the Health People 2020 goal of 60%.2 Patients treated in the rheumatology and MM clinics were immunized at 21.6% and 23.4%3, respectively, prior to the intervention.
Intervention: Clinical Education
The interprofessional project team included members trained in medicine, infectious diseases, quality improvement methodology, health literacy and continuing education. The team first developed educational sessions for the healthcare team to improve their ability to use ACIP guidelines to immunize immunocompromised patients with pneumococcal vaccine. These sessions also introduced new patient education resources described below.
The content was presented at two accredited UAMS Grand Rounds sessions, reaching internal medicine and oncology practitioners. Presentations were recorded to provide a digital archive for new clinical staff and for those in need of future review.
Team members provided serial informal educational sessions and updates on vaccination rates to clinical staff, providers and learners in the MM and rheumatology clinics to reinforce the need to immunize, problem solve and encourage preventive immunization as a key component to ongoing patient care.
Intervention: Patient Education
A patient education handout was developed using the Health Belief model as a guide for content (perceived risk, severity of disease, perceived barriers and benefits to vaccination). The content was formally tested by the health literacy team with validated readability formulas, the Patient Educational Materials Assessment Tool, and three field testing sessions inclusive of English and Spanish speakers with documented risk for limited health literacy. This handout was used in the clinics to facilitate discussions with the patients who needed to be vaccinated.
Intervention: Systems Changes
Clinic system improvements were implemented in the first three months of the project to facilitate the healthcare team’s ability to assess the need for the pneumococcal vaccine in immunocompromised patients ages 19–64. These system improvements began with use of vaccine standing orders.
Best practice advisories were integrated into the electronic medical record system to serve as reminders to the clinical staff to check vaccination status and to access the patient education materials as needed.
A major system change was implemented in the MM clinic to facilitate vaccination of this patient population. Prior to this project, the MM patients were sent to another clinic for vaccinations, rather than vaccinated at their MM clinic visit. Multiple patients did not complete vaccinations, due to the burden of waiting at another appointment. To solve the system issue, a clinic room with a vaccine refrigerator dedicated to vaccine administration was established in the MM clinic. This was considered a great long-term improvement that will benefit patients for years.
Accomplishments
Rates of vaccine protection nearly doubled in a six-month period, going from 21.6% to 41% in the rheumatology clinic and from 23.4% to 46% in the MM clinic. They continued to increase until disrupted by COVID-19.
Our team’s approach could be replicated by others. Approximately 10 million American adults are considered immunocompromised and would benefit from widespread launch of similar programming.4
Dissemination
A poster was accepted by and presented at the Institute for Healthcare Advancement (IHA) 19th Annual Health Literacy Conference in July 2020. The theme was health equity and disparities in the time of COVID-19. The poster won second place overall for poster presentations.
Another poster presentation was accepted for the April 2021 72nd Annual Conference of the Society for Public Health Education, Virtual Conference, entitled “Clinical QI Story: Improving Pneumococcal Vaccine Rates in Immunocompromised Adults With Help From Health Behavior Theory and Plain Language.”
Impact of COVID
COVID-19 brought a halt to the project’s short-term impact while the clinics were closed. Since reopening, the clinical staff and our project physicians have been focused on COVID-19 response and its impacts on patient care. However, the systems changes to integrate this work into the electronic medical record, provide appropriate facilities and equipment for vaccine storage and make actionable patient education materials available are investments likely to facilitate renewed and sustained impact as clinical operations return to a pre-COVID state.
We believe the interventions would easily translate to the COVID-19 vaccine dissemination, and our Center for Health Literacy has been preparing patient education materials in a similar manner.
1Williams WW, Lu P, O’Halloran A, et al. Surveillance of Vaccination Coverage among Adult Populations — United States, 2015. MMWR Surveill Summ 2017;66(No. SS-11):1–28.
2 https://www.healthypeople.gov/2020/topics- objectives/topic/immunization-and-infectious-diseases/objectives
3Institutional data, University of Arkansas for Medical Sciences
4https://jamanetwork.com/journals/jama/fullarticle/2572798